AP Syllabus focus:
‘The epidemiological transition explains causes of changing death rates, including shifts in disease and health conditions.’
The epidemiological transition outlines how dominant causes of death change as societies develop, shaping shifting death rates and influencing population patterns across different stages of economic and social progress.
Epidemiological Transition: Overview
The epidemiological transition is a model describing how patterns of mortality evolve alongside economic development, medical advancements, and social transformation. It complements the Demographic Transition Model (DTM) by explaining why death rates rise or fall at different stages. While the DTM focuses on fertility and mortality trends, the epidemiological transition adds essential detail about the underlying disease environments, health conditions, and technological changes that drive mortality patterns.
Epidemiological Transition: A model explaining long-term shifts in the patterns and causes of death, especially the transition from infectious to chronic, degenerative diseases as societies develop.
Understanding this transition helps geographers interpret differences in mortality between regions at varying levels of development, as well as changes within a single country over time.
Stage 1: Pestilence and Famine
In the earliest period of human history and in pre-industrial societies, death rates are extremely high and fluctuate widely. Societies in this stage typically experience:
Frequent epidemics caused by contagious diseases such as cholera, smallpox, and plague.
High infant and child mortality, as infectious diseases disproportionately affect younger populations.
Food scarcity and widespread malnutrition, which increase vulnerability to disease.
Environmental hazards, including poor sanitation and contaminated water sources.
Mortality in this stage is driven primarily by infectious, parasitic, and nutritional deficiency diseases, leading to short life expectancy and slow or stagnant population growth.
Stage 2: Receding Pandemics
As sanitation improves and societies begin early industrialization, death rates decline. This transition often corresponds with Stage 2 of the DTM, where falling mortality drives rapid population growth. Key characteristics include:
Improvements in public health, such as cleaner water supplies and better sewage infrastructure.
Declines in epidemic frequency and severity, with fewer large-scale outbreaks.
Rising life expectancy, though disparities remain between urban and rural areas.
Continued presence of infectious diseases, but with reduced mortality due to basic medical interventions.
Pandemic: A widespread disease outbreak affecting populations across countries or continents.
Even though pandemics become less lethal, they may still disrupt social and economic systems. The reduction in mortality is often uneven, with poorer communities benefiting later than wealthier ones.
Stage 3: Degenerative and Chronic Diseases
In more industrialized societies, mortality patterns shift from infectious diseases to chronic, long-term illnesses. This stage reflects ongoing social and economic development and a major transformation in health outcomes. Populations experience:
Lower death rates overall, with longer average life expectancy.
Rising prevalence of degenerative diseases such as heart disease, cancer, and stroke.
Lifestyle-related health issues, including those linked to diet, physical inactivity, and stress.
Continued medical advancements that extend life but may not eliminate chronic disease risks.
These changes reflect enhanced standards of living, improved nutrition, and advanced medical care. However, the aging of the population increases the proportion of deaths from chronic conditions.
Stage 4: Delayed Degenerative Diseases
With further technological and medical advancement, societies enter a stage where degenerative diseases remain common but are experienced later in life. This stage is marked by:
Very high life expectancy, often exceeding 80 years.
Medical innovations that delay the onset or reduce mortality from chronic diseases.
Declines in deaths from smoking-related illnesses, heart disease, and some cancers due to public health interventions.
Greater emphasis on preventive care, including screenings, vaccinations, and health education.
While chronic diseases still account for most deaths, their severity and timing change, allowing people to live longer, healthier lives.
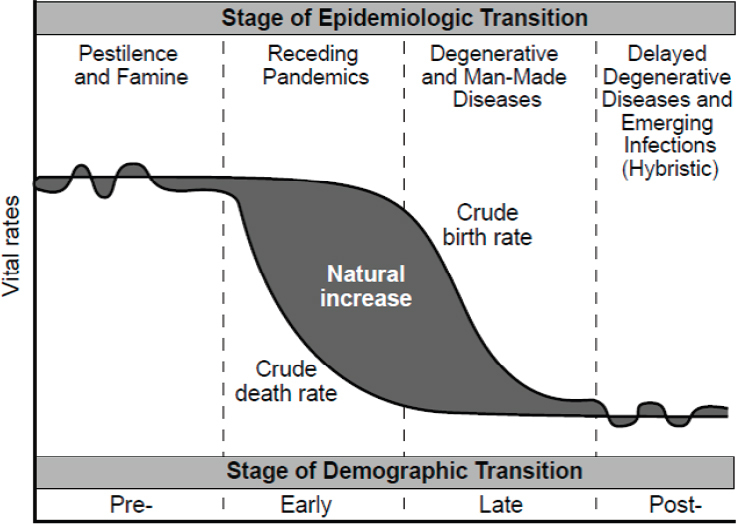
A demographic and epidemiologic transition framework illustrating changes in crude birth and death rates alongside shifts from infectious to chronic diseases. The shaded region shows natural increase and highlights how mortality decline interacts with changing disease patterns. The diagram includes additional demographic detail beyond the AP syllabus but directly supports understanding of changing death rates. Source.
Stage 5: Possible Reemergence of Infectious Diseases
Some scholars propose a fifth stage characterized by the reemergence of infectious diseases and new mortality challenges that may raise death rates in some regions. Contributing factors include:
Antibiotic resistance, which reduces the effectiveness of medical treatments.
Globalization, enabling rapid disease spread through travel and trade.
Urban overcrowding and sanitation challenges, especially in rapidly growing cities in developing regions.
Novel pathogens such as COVID-19, which can cause significant mortality even in developed societies.
Climate change, influencing the spread of vector-borne diseases like malaria and dengue.
This stage illustrates that mortality transitions are not strictly linear; new health threats can disrupt previously stable patterns.
Linking Epidemiological Transition to Changing Death Rates
The epidemiological transition directly shapes death rates by altering the predominant causes of mortality.
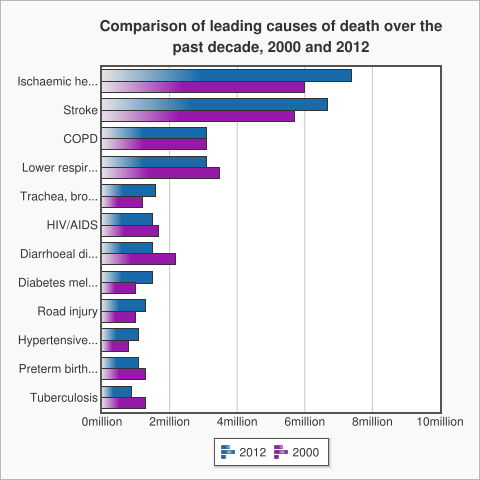
A bar chart comparing global leading causes of death in 2000 and 2012, showing the increasing dominance of noncommunicable diseases such as stroke and ischemic heart disease. These trends reflect the later stages of the epidemiologic transition, where chronic conditions become the main drivers of mortality. The chart includes additional detail beyond the AP syllabus but effectively illustrates the shift away from infectious causes. Source.
As societies advance through stages, death rates fall due to declines in infectious diseases and improvements in nutrition, sanitation, and health care. Later stages feature stable, low death rates, but shifting causes of mortality toward chronic conditions. Across all stages, the model highlights how disease environments, medical technologies, social behaviors, and economic development interact to influence mortality trends at varying scales.
FAQ
High-income countries typically progress through the stages earlier, experiencing a rapid decline in infectious diseases due to early investments in sanitation, vaccination, and medical technology.
Low-income countries often show mixed patterns, where infectious diseases remain significant while chronic diseases simultaneously rise.
This creates a double burden of disease, making health planning more complex.
Urbanisation accelerates the decline of infectious diseases by improving access to healthcare, clean water, and sanitation.
However, it also contributes to the rise of chronic diseases through lifestyle changes such as reduced physical activity, processed-food consumption, and increased exposure to pollution.
Reappearance often results from:
Antibiotic resistance
Global travel spreading pathogens quickly
New disease strains
Climate-related changes in disease vectors
These factors allow infectious diseases to emerge even in highly developed health systems.
Early stages require investment in public health infrastructure, sanitation, vaccines, and maternal and child health.
Later stages shift spending toward long-term care, chronic disease management, screening programmes, and elderly care, reflecting the dominance of degenerative conditions.
Governments must also budget for emerging infectious threats, particularly in a globally connected world.
Countries in early stages show high mortality, short life expectancy, and young population structures influenced by deaths from infectious diseases.
Later stages feature low mortality, long life expectancy, and ageing populations due to the predominance of chronic, non-communicable conditions.
These patterns help geographers interpret health transitions even without detailed medical data.
Practice Questions
Question 1 (1–3 marks)
Identify one characteristic of Stage 2 (Receding Pandemics) in the epidemiological transition and explain how it influences death rates.
Question 1 (1–3 marks)
1 mark for identifying a correct characteristic of Stage 2, such as improved sanitation, declining frequency of epidemics, or early medical advancements.
1–2 marks for explaining how this characteristic reduces death rates, such as fewer infectious disease outbreaks or improved survival due to cleaner water and basic healthcare.
(Max 3 marks)
Question 2 (4–6 marks)
Using the epidemiological transition model, analyse how the dominant causes of death change as a country progresses from Stage 1 to Stage 4. In your answer, refer to shifts in disease types and broader social or economic factors.
Question 2 (4–6 marks)
Award marks for the following points:
1 mark for describing mortality in Stage 1 (high death rates due to infectious, parasitic, and nutritional deficiency diseases).
1 mark for identifying the shift in Stage 2 (declining infectious diseases due to sanitation and public health improvements).
1 mark for explaining the rise of chronic and degenerative diseases in Stage 3.
1 mark for noting delayed degenerative diseases in Stage 4, with increased life expectancy due to advanced medical care.
Up to 2 additional marks for linking these shifts to social or economic development, such as improved living standards, changing lifestyles, or advances in technology and healthcare.
(Max 6 marks)

