OCR Specification focus:
‘Describe how hormones and nerves alter heart rate; compare skeletal, involuntary and cardiac muscle; neuromuscular junctions; sliding filament contraction; ATP role and creatine phosphate supplying ATP.’
Heart Rate Control and Muscle Contraction
The control of heart rate and muscle contraction integrates nervous, hormonal, and biochemical mechanisms to ensure efficient responses to changing physiological demands in animals.
Control of Heart Rate
The Role of the Heart’s Pacemaker
The sinoatrial node (SAN), located in the wall of the right atrium, initiates electrical impulses that set the rhythm of the heartbeat. This intrinsic rhythm is known as the myogenic rate. The SAN’s impulses spread across the atria, causing contraction, before reaching the atrioventricular node (AVN), which delays transmission to ensure the atria empty before ventricular contraction.
Nervous Control via the Autonomic Nervous System
Heart rate is regulated by the autonomic nervous system (ANS), which operates involuntarily through two opposing branches:
Sympathetic nervous system: increases heart rate through the accelerator nerve.
Parasympathetic nervous system: decreases heart rate through the vagus nerve.
Signals from these nerves act on the SAN to alter the frequency of depolarisation and therefore modify the cardiac cycle.
Autonomic Nervous System: The part of the peripheral nervous system that regulates involuntary physiological functions such as heart rate, digestion, and respiration.
Medulla Oblongata and Chemoreceptors
The medulla oblongata in the brainstem coordinates cardiac control by processing inputs from chemoreceptors and baroreceptors:
Chemoreceptors in the carotid arteries and aorta detect changes in carbon dioxide concentration and pH. An increase in CO₂ leads to a decrease in blood pH, stimulating the medulla to increase sympathetic stimulation of the SAN, raising heart rate.
Baroreceptors detect blood pressure changes. High pressure triggers parasympathetic stimulation to reduce heart rate; low pressure causes sympathetic stimulation to raise it.
Hormonal Influence
Adrenaline, secreted by the adrenal medulla, binds to receptors on the SAN, increasing the rate of depolarisation. This prepares the body for “fight or flight” by increasing oxygen delivery to muscles. Noradrenaline has a similar excitatory effect.
Types of Muscle Tissue
Overview
There are three major muscle types in animals: skeletal, cardiac, and smooth (involuntary). Each has distinct structural and functional characteristics.
Skeletal muscle: under voluntary control, responsible for body movement.
Cardiac muscle: involuntary and myogenic, forming the heart wall.
Smooth muscle: involuntary, found in organs such as the gut and blood vessels.
Skeletal Muscle
Skeletal (striated) muscle is made up of long multinucleate fibres containing myofibrils, which are the contractile units. It contracts rapidly but fatigues relatively quickly.
Myofibril: A microscopic thread-like structure within muscle fibres containing the contractile proteins actin and myosin responsible for muscle contraction.
Involuntary (Smooth) Muscle
Smooth muscle cells are spindle-shaped and uninucleate, lacking striations. Contraction is slow, sustained, and not under conscious control, allowing processes like peristalsis and vasoconstriction.
Cardiac Muscle
Cardiac muscle shares properties of both skeletal and smooth muscle:
Myogenic activity enables autonomous contraction.
Intercalated discs connect cells, allowing coordinated contraction through electrical coupling.
Contraction is rhythmic, resistant to fatigue, and vital for continuous pumping.
Neuromuscular Junctions
Structure and Function
A neuromuscular junction (NMJ) is a specialised synapse between a motor neurone and a skeletal muscle fibre, enabling the transmission of nerve impulses into mechanical contraction.

Schematic of a neuromuscular junction showing presynaptic vesicle fusion and acetylcholine (ACh) release, receptor binding on the sarcolemma, and the resulting depolarisation that initiates contraction. Labels highlight the axon terminal, synaptic cleft, and muscle fibre interface, matching the described process. Source.
When an action potential reaches the axon terminal:
Calcium ions enter through voltage-gated channels.
Synaptic vesicles release acetylcholine (ACh) into the synaptic cleft.
ACh binds to receptors on the muscle fibre’s sarcolemma, causing depolarisation.
The impulse spreads through T-tubules, triggering calcium ion release from the sarcoplasmic reticulum.
Calcium initiates the sliding filament mechanism.
Acetylcholine: A neurotransmitter that diffuses across synapses or neuromuscular junctions to trigger an action potential in a post-synaptic membrane or muscle fibre.
The Sliding Filament Mechanism
Contractile Proteins
Muscle contraction depends on the interaction between actin (thin) and myosin (thick) filaments within the sarcomere.
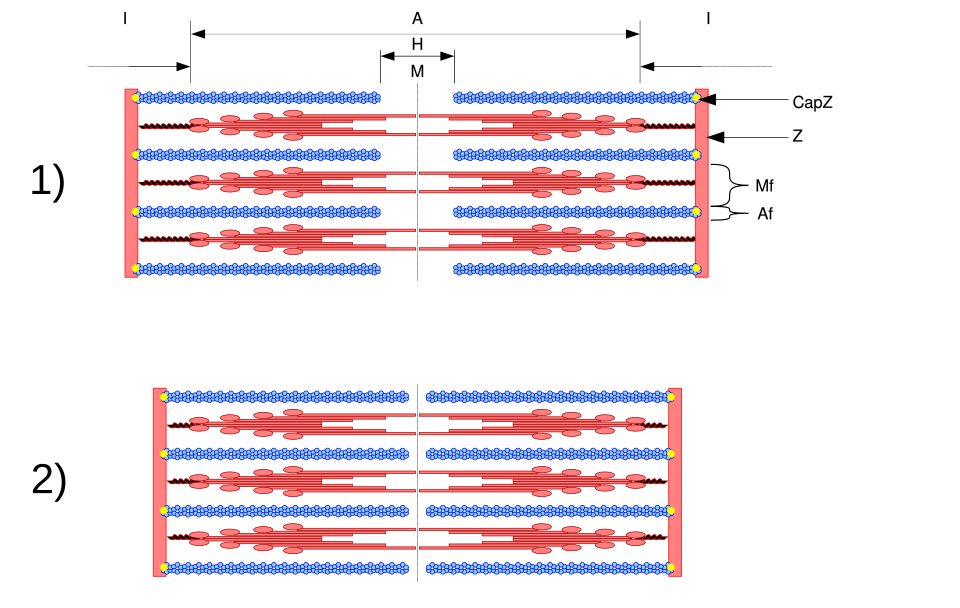
Labeled sarcomere diagram indicating Z-lines, I-band, A-band, H-zone, M-line, and the relative positions of actin and myosin. Use this to reinforce that I-band and H-zone shorten during contraction while the A-band length remains constant. Contains general structural labels only. Source.
Calcium ions bind to troponin, causing tropomyosin to move and expose binding sites on actin.
Myosin heads form cross-bridges with actin.
The myosin heads pivot, pulling actin filaments inward — the power stroke.
ATP binds to myosin, breaking the cross-bridge.
Hydrolysis of ATP resets the myosin head for another cycle.
Sarcomere Structure
The sarcomere is the functional unit of a myofibril, defined by Z-lines. During contraction:
I-band and H-zone shorten.
A-band remains the same length.
Sarcomere: The repeating unit of a myofibril bounded by Z-lines, within which actin and myosin filaments slide to produce muscle contraction.
Energy Supply for Muscle Contraction
ATP and its Functions
ATP is essential for:
Cross-bridge formation and detachment.
Active transport of calcium ions back into the sarcoplasmic reticulum.
Maintenance of the resting potential in muscle fibres.
When oxygen supply is sufficient, ATP is generated via aerobic respiration in mitochondria.
Anaerobic Pathways and Creatine Phosphate
During intense activity, oxygen may become limited. ATP is then produced through:
Anaerobic respiration (glycolysis), generating lactic acid.
The creatine phosphate system, which provides a rapid but short-term supply of ATP.
EQUATION
—-----------------------------------------------------------------
Creatine Phosphate Reaction (Phosphocreatine system):
Creatine phosphate + ADP → Creatine + ATP
Creatine phosphate = A high-energy compound that donates phosphate to ADP.
ADP (adenosine diphosphate) = Molecule that accepts phosphate to form ATP.
ATP (adenosine triphosphate) = The primary energy currency of cells.
—-----------------------------------------------------------------
This mechanism supports muscle contraction during brief bursts of high-intensity activity while aerobic pathways recover.
FAQ
The baroreceptors in the aortic arch and carotid sinus detect the degree of stretch in arterial walls.
When blood pressure rises, baroreceptors increase their firing rate, sending impulses to the cardiac centre in the medulla, which activates the parasympathetic vagus nerve to reduce SAN activity and slow heart rate.
When blood pressure falls, fewer impulses are sent, prompting the sympathetic accelerator nerve to increase SAN depolarisation and raise heart rate.
This continuous feedback allows moment-to-moment cardiovascular stability.
Cardiac muscle has a rich blood supply, a high mitochondrial density, and continuous aerobic metabolism.
It operates almost exclusively using oxidative phosphorylation, ensuring efficient ATP production.
Myoglobin concentration is high, maintaining oxygen availability even during brief reductions in blood flow.
The presence of intercalated discs allows electrical coupling, ensuring coordinated contraction and recovery across the myocardium.
These features prevent the oxygen debt that leads to skeletal muscle fatigue.
After acetylcholine (ACh) binds to receptors, it is rapidly broken down by acetylcholinesterase in the synaptic cleft.
This enzyme converts ACh into choline and acetate, which are reabsorbed into the presynaptic terminal to form new ACh molecules.
By removing ACh, the sarcolemma repolarises, voltage-gated calcium channels close, and calcium ions are pumped back into the sarcoplasmic reticulum.
This prevents sustained depolarisation and ensures precise, controlled contractions.
Each myosin head contains two functional sites:
A binding site for actin.
An ATPase site, which hydrolyses ATP to ADP and Pi.
When ATP binds, the myosin head detaches from actin. Hydrolysis re-cocks the head into a high-energy position.
Upon binding to a new actin site, Pi release triggers the power stroke, pulling the actin filament.
ADP is then released, and a new ATP molecule reinitiates the cycle.
This structural design ensures directional, cyclic movement at the molecular level.
When oxygen supply is limited, muscles shift to anaerobic ATP sources:
Creatine phosphate system: transfers phosphate directly to ADP, rapidly generating ATP for up to 10 seconds.
Anaerobic glycolysis: breaks down glucose into pyruvate, forming ATP and producing lactic acid as a by-product.
Creatine phosphate provides the fastest ATP regeneration, while glycolysis sustains output slightly longer.
Both systems allow continued contraction until aerobic metabolism can resume or energy stores are depleted.
Practice Questions
Question 1 (3 marks)
Describe how the autonomic nervous system controls changes in heart rate in response to an increase in carbon dioxide concentration in the blood.
Mark scheme:
(1 mark) Increased carbon dioxide concentration lowers blood pH, detected by chemoreceptors in the carotid arteries or aorta.
(1 mark) Impulses are sent to the medulla oblongata, which increases activity in the sympathetic nervous system.
(1 mark) The accelerator nerve stimulates the sinoatrial node (SAN) to increase the rate of depolarisation and therefore increase heart rate.
Question 2 (6 marks)
Explain the sequence of events that occurs at the neuromuscular junction leading to muscle contraction, and describe the role of ATP during the contraction process.
Mark scheme:
(1 mark) Arrival of an action potential at the axon terminal causes calcium ions to enter through voltage-gated channels.
(1 mark) Synaptic vesicles release acetylcholine (ACh) into the synaptic cleft by exocytosis.
(1 mark) ACh binds to receptors on the sarcolemma, causing depolarisation that spreads through T-tubules.
(1 mark) Depolarisation triggers calcium ion release from the sarcoplasmic reticulum into the cytoplasm.
(1 mark) Calcium ions bind to troponin, causing tropomyosin to move and expose actin binding sites, enabling cross-bridge formation with myosin.
(1 mark) ATP is required to detach myosin heads from actin, re-cock the heads for the next power stroke, and actively transport calcium ions back into the sarcoplasmic reticulum at the end of contraction.

