OCR Specification focus:
‘Describe A-scan and B-scan ultrasound techniques and typical uses.’
Ultrasound imaging employs reflected high-frequency sound to determine internal structures. A-scan and B-scan modes provide distinct methods for recording returning echoes, enabling clinicians to interpret depth information and create visual representations.
A-scan Ultrasound
A-scan ultrasound is a one-dimensional measurement technique that records the amplitude of returning ultrasound pulses against time, allowing precise distance information within the body. It is essential for applications requiring accurate depth measurements rather than image formation.
Nature of A-scan Data
When a short ultrasound pulse is transmitted into the body, echoes return whenever the wave encounters a boundary between two tissues with different acoustic impedances. The time taken for each echo to return corresponds to the depth of that reflecting boundary. This measurement technique forms the foundation of A-scan operation.
A-scan (Amplitude scan): A one-dimensional ultrasound technique that displays echo amplitude as a function of time to determine the depth of internal boundaries.
An A-scan trace appears as a series of vertical spikes. Each spike’s position on the time axis indicates the location of a boundary, while its height indicates the strength of the reflection. Because the ultrasound pulse is narrow and well-timed, the display gives highly accurate axial information.
On the screen, an A-scan appears as a series of vertical spikes plotted against distance along a single line into the body.
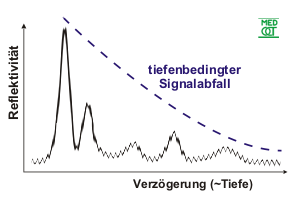
A-mode ultrasound display showing echo amplitude as vertical spikes against depth. Each spike represents a tissue boundary along the ultrasound beam, illustrating how A-scans measure distances rather than form an image. Axis labels are in German, but students should focus on the relationship between spike height and reflecting surfaces rather than the specific wording. Source.
Because the ultrasound pulse is narrow and well-timed, the display gives highly accurate axial information.
Process of A-scan Operation
A typical A-scan involves the following steps:
Pulse emission from a piezoelectric transducer into the patient.
Propagation of ultrasound through soft tissues until encountering a boundary.
Reflection of part of the wave back to the transducer, generating an electrical signal.
Display of echo amplitude versus time, forming a depth profile.
Interpretation by clinicians to determine distances, commonly for eye measurements.
Normal operation requires the speed of ultrasound in the medium to be known so that time-of-flight can be converted into distance. For example, soft tissue uses an approximate speed of 1.54 × 10³ m s⁻¹. This is crucial for ophthalmology, where A-scan precision helps determine intraocular distances for lens power calculations.
A-scans do not provide spatial images. Instead, they act as accurate measuring tools. Their simplicity makes them reliable for routine biometry, especially in situations where a full image is unnecessary.
B-scan Ultrasound
While A-scan focuses on depth measurement, B-scan ultrasound provides a two-dimensional brightness-based image. Each returning echo is represented as a dot, and the dot’s brightness corresponds to the strength of the reflection. Sweeping the transducer builds up a cross-sectional image.
Formation of B-scan Images
In B-scan mode, each ultrasound pulse generates a line of depth information equivalent to an A-scan, but the system assigns a brightness level to each echo instead of a spike. The machine then plots this brightness at the correct position on the screen. As the transducer is moved, a two-dimensional image emerges.
B-scan (Brightness scan): A two-dimensional ultrasound imaging technique in which echoes are displayed as dots with brightness proportional to echo amplitude, forming cross-sectional images.
This brightness-based representation allows clinicians to view the shape, size, and internal arrangement of organs. As the image is built line by line, the technique creates a recognisable diagnostic picture, similar in appearance to other medical imaging modalities but using harmless ultrasound instead of ionising radiation.
In B-scan mode, each returning echo controls the brightness of a dot on the screen, building up a two-dimensional cross-sectional image in real time.

B-mode ultrasound image showing a cross-section of a human eye, with the lens, vitreous humour, and hyaloid canal labelled. The varying brightness represents different echo strengths, illustrating how B-scan converts echo amplitude into a grey-scale image. This particular scan is of a fetal eye in utero, which goes beyond the A-level syllabus but still clearly demonstrates the principle of B-scan imaging. Source.
The resulting image is typically displayed as a greyscale map in which brighter points correspond to stronger reflections, such as those from bone or organ boundaries.
Method of Acquiring a B-scan
A B-scan requires coordinated transducer movement and data processing:
Emission and detection of pulses similar to A-scan operation.
Conversion of echo amplitude into pixel brightness.
Angular or linear sweeping of the transducer across the region of interest.
Real-time assembly of brightness dots on a display to construct a cross-section.
Continuous updating of the image as the transducer is repositioned.
The resulting image is typically displayed as a greyscale map in which brighter points correspond to stronger reflections, such as those from bone or organ boundaries.
Uses of B-scan Imaging
Because B-scan produces a cross-section rather than a single measurement, it is suited to applications where visual interpretation is essential. Common uses include:
Abdominal scanning, enabling clinicians to view organ outlines.
Obstetric imaging, allowing safe visualisation of the foetus.
Soft-tissue assessment, particularly when mapping fluid regions or masses.
Ophthalmic diagnostics, where structural abnormalities of the eye can be detected.
B-scan’s ability to provide intuitive visual information makes it central to modern clinical practice. Its safety, portability, and absence of ionising radiation support widespread routine use.
Comparing A-scan and B-scan Techniques
Although both modes rely on the same physical principles of ultrasound reflection, their outputs serve different clinical purposes.
Key Differences
Dimensionality:
A-scan yields a one-dimensional depth profile.
B-scan constructs a two-dimensional image.
Representation:
A-scan uses spikes to show echo amplitudes.
B-scan uses varying brightness of dots.
Primary use:
A-scan excels in precise distance measurement.
B-scan provides structural imaging.
Understanding these differences helps students appreciate the complementary roles of each mode.
FAQ
Higher frequencies produce better resolution because the wavelength is shorter, allowing smaller structures to be distinguished.
However, high-frequency waves attenuate more quickly, limiting penetration depth. Lower frequencies penetrate deeper but give poorer resolution.
In practice:
A-scans often use higher frequencies when measuring small internal distances, such as in ophthalmology.
B-scans balance resolution and penetration to create usable cross-sectional images of organs.
Electronic steering allows rapid changes in beam direction without mechanical movement.
This enables:
Faster image acquisition
Reduced motion blur
More consistent line spacing
Improved reliability due to fewer moving parts
It also supports compound imaging, where beams from multiple angles provide clearer boundaries and reduced speckle.
Brightness is influenced not only by boundary reflections but also by internal scattering.
Factors include:
Tissue density variations
Presence of small reflectors such as fibres or microcalcifications
Angle between the ultrasound beam and structures
Attenuation causing distant echoes to appear weaker even if the boundary is strong
Machine settings such as gain and dynamic range also affect perceived brightness.
A-scans rely on converting time-of-flight into depth, so timing accuracy is essential.
Precision is ensured through:
Stable high-frequency clock circuits
Consistent pulse generation
Fast analogue-to-digital conversion
Calibration using materials of known acoustic properties
Minor timing errors can cause significant depth inaccuracies, especially when measuring small anatomical features.
Frame rate depends on how quickly multiple lines of ultrasound data can be collected.
Limitations arise from:
Speed of sound in tissue, which restricts how fast echoes return
Number of A-lines required for each frame
Processing time for brightness mapping
Any mechanical sweeping of the transducer
A lower frame rate can make moving structures (such as a beating heart) appear blurred or distorted, reducing diagnostic reliability.
Practice Questions
Question 1 (2 marks)
State what is meant by an A-scan in ultrasound imaging and describe one typical medical use of this mode.
Question 1 (2 marks)
1 mark: Identifies that an A-scan is a one-dimensional ultrasound display showing echo amplitude against time or depth.
1 mark: Gives a correct typical medical use, e.g. measuring intraocular distances, eye biometry, or determining distances within soft tissues.
Question 2 (5 marks)
A clinician uses B-scan ultrasound to examine soft tissue.
(a) Explain how a B-scan forms a two-dimensional image from ultrasound reflections.
(b) Discuss why B-scan is more suitable than A-scan for diagnosing structural abnormalities in organs.
Your answer should refer to the information provided by each mode.
Question 2 (5 marks)
1 mark: States that B-scan uses many ultrasound pulses or A-lines to create an image.
1 mark: Explains that each echo is represented by a dot whose brightness corresponds to echo amplitude.
1 mark: Describes that sweeping or moving the transducer builds up a cross-sectional (two-dimensional) image.
1 mark: Explains that B-scan provides spatial information or organ structure rather than only depth information.
1 mark: States that B-scan is better for diagnosing abnormalities because it shows shapes, boundaries, and internal features, allowing visual interpretation.

