OCR Specification focus:
‘Use intensity reflection coefficient R = [(Z2 − Z1)/(Z2 + Z1)]²; explain gel for impedance matching.’
Ultrasound imaging depends critically on how sound waves behave at boundaries between different tissues, making reflection control and effective coupling essential for producing diagnostically useful images. These notes explore how acoustic impedance differences, boundary interactions, and coupling agents influence reflected intensity in medical ultrasound systems.
Reflection of Ultrasound at Tissue Boundaries
When an ultrasound pulse encounters an interface between two media, part of the incident wave is reflected and the remainder is transmitted. The proportion reflected is governed primarily by the acoustic impedance difference across the boundary. Large differences create strong reflections, while small differences promote transmission.
Reflection occurs whenever ultrasound encounters a boundary between two materials with different acoustic impedances.
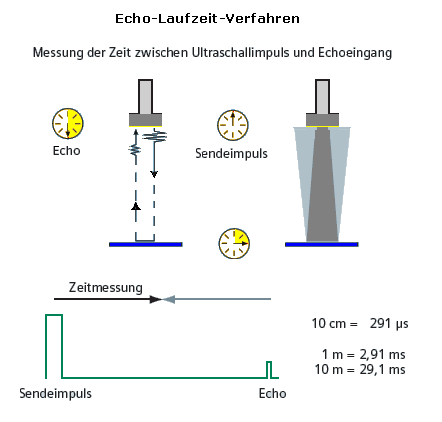
Diagram showing how an ultrasound beam partly reflects and partly transmits at internal boundaries within a material. The German labels provide extra context, but the key concept is the generation of echoes at impedance changes. Source.
Acoustic Impedance (Z): The product of a medium’s density and the speed of sound within it.
Because various tissues—such as soft tissue, fat, and bone—have differing densities and sound speeds, their acoustic impedances vary. This means ultrasound reflection occurs naturally inside the body and can be exploited to form images. However, these reflections must be controlled deliberately: some are useful, while others (such as reflections at the skin surface) can prevent energy from entering the body effectively.
Ultrasound scanners rely on predictable reflection patterns, so the ability to quantify reflected intensity is essential. The intensity reflection coefficient, given in the OCR specification, provides this quantitative link.
EQUATION
—-----------------------------------------------------------------
Intensity Reflection Coefficient (R) = [(Z₂ − Z₁)/(Z₂ + Z₁)]²
Z₁ = Acoustic impedance of the first medium (kg m⁻² s⁻¹)
Z₂ = Acoustic impedance of the second medium (kg m⁻² s⁻¹)
R = Fraction of incident intensity reflected at the boundary (dimensionless)
—-----------------------------------------------------------------
This equation shows that even modest impedance differences can generate perceptible reflections. For example, interfaces between muscle and fat produce small reflections, while the boundary between soft tissue and bone produces very strong reflections that can obscure deeper structures. Understanding these relationships allows clinicians to interpret image brightness and contrast correctly.
Why Reflection Matters for Medical Imaging
Reflections enable the formation of echoes, which are detected by the transducer and used to construct A-scan and B-scan images. Brightness and structure in these images correspond to the strength and timing of echoes. Key implications include:
High reflection interfaces (e.g., tissue–bone):
Produce bright signals
Limit penetration depth
May create acoustic shadows
Low reflection interfaces (e.g., between similar soft tissues):
Provide subtle backscatter
Allow visualisation of internal soft-tissue organisation
Ultrasound systems therefore balance pulse power, frequency, and signal processing to extract maximal information from reflected waves while minimising artefacts.
Coupling Ultrasound into the Body
A major challenge arises at the first boundary encountered: the air–skin interface. Air has a very low acoustic impedance, whereas skin has a significantly higher one. Substituting these values into the reflection coefficient equation shows that almost all the ultrasound intensity would be reflected, leaving very little energy available to penetrate the body.
To overcome this, ultrasound examinations use a coupling gel. The physical function of this gel is closely tied to the specification requirement to “explain gel for impedance matching.”
A coupling gel is spread on the patient’s skin to match acoustic impedances and remove air gaps between the transducer and the body surface.

A clinical ultrasound system positioned next to an examination bed. During imaging, coupling gel would be applied to ensure effective transmission of ultrasound into the body. The room furnishings shown provide additional context beyond the syllabus but illustrate the real environment where reflection and coupling principles apply. Source.
Purpose and Function of Coupling Agents
Coupling gels are formulated to:
Eliminate air gaps between the transducer and skin
Reduce impedance mismatch so that more of the ultrasound wave enters the body
Enhance transmission quality, thereby improving signal-to-noise ratio
Provide consistent acoustic contact, allowing smooth movement of the transducer
Impedance Matching: The process of reducing the difference in acoustic impedance between two media to maximise transmission of ultrasound.
Coupling gels typically contain water-based components because water’s acoustic impedance is much closer to that of soft tissue than air. This shift dramatically reduces reflected intensity at the skin surface.
Between definition blocks and technical discussion, students should appreciate that coupling is not merely a practical step but one grounded in wave physics.
How Coupling Improves Image Quality
Effective coupling enables:
Stronger transmitted pulses, providing deeper penetration
Clearer, less noisy echoes, improving diagnostic accuracy
Stable contact, reducing artefacts related to inconsistent pressure or movement
By minimising the dominant unwanted reflection at the air–skin boundary, the gel ensures that reflections recorded by the scanner originate mainly from internal tissue interfaces, where clinically relevant information resides.
Interpreting Reflection in Clinical Imaging
Ultrasound practitioners must recognise how variations in tissue properties influence the reflected intensity pattern. Useful imaging outcomes rely on:
Appropriate gel application to ensure uniform coupling
Selecting suitable frequency (higher for superficial detail, lower for deep penetration)
Understanding tissue boundaries, including those likely to generate strong reflections
Reflection characteristics help clinicians identify structures such as organs, cysts, tumours, blood vessel walls, and foetal anatomy. The careful interpretation of reflected signals—guided by acoustic impedance differences—underpins the diagnostic power of ultrasound imaging and emphasises why reflection and coupling are core parts of the OCR specification for medical physics.
FAQ
Reflection depends not only on the impedance difference but also on geometry. At oblique angles, part of the wave may refract into the second medium, reducing the proportion reflected back toward the transducer.
At larger angles, refraction becomes more significant and can redirect transmitted energy away from the detector. This is why medical imaging works best when the transducer is held so that ultrasound strikes tissue boundaries close to normal incidence.
If a boundary is smooth at the scale of the wavelength, reflections are mostly specular, returning energy in a single direction.
A rough boundary produces diffuse reflection, spreading the returned echoes over a wider range of angles.
This can reduce the amplitude of the signal detected by the transducer.
It can increase image speckle, affecting clarity.
Higher-frequency waves have shorter wavelengths, making them more responsive to small structural and impedance variations.
This means high-frequency ultrasound produces stronger echoes from fine boundaries but also attenuates more strongly, limiting penetration depth. Lower frequencies generate weaker reflections from small impedance steps but penetrate deeper into tissue.
Although water is often used as an acoustic reference, commercial gels include thickeners and polymers that adjust viscosity and acoustic impedance.
These additives:
Prevent the gel from running off the skin
Improve adhesion between transducer and skin
Tune the impedance slightly closer to soft tissue to maximise transmission
This makes gels more practical and acoustically effective than pure water.
Even a very thin air layer between the transducer and skin produces almost total reflection, because air’s impedance is extremely low.
Insufficient gel can cause:
Flickering or noisy echoes
Patchy loss of image regions
Reduced penetration
The gel must completely fill microscopic gaps, not just visibly coat the surface, to prevent high-reflection air pockets.
Practice Questions
Question 1 (2 marks)
Ultrasound imaging requires the use of a coupling gel between the transducer and the patient’s skin.
Explain why this gel is necessary for effective ultrasound transmission into the body.
Question 1 (2 marks)
Gel eliminates air gaps between transducer and skin. (1 mark)
Reduces the acoustic impedance mismatch so more ultrasound enters the body. (1 mark)
Question 2 (5 marks)
An ultrasound wave travels through soft tissue and encounters a boundary with bone.
(a) Explain why a strong reflection occurs at this boundary.
(b) State the equation for the intensity reflection coefficient and describe what each term represents.
(c) Discuss one implication of this strong reflection for medical ultrasound imaging.
Question 2 (5 marks)
(a)
Large difference in acoustic impedance between soft tissue and bone. (1 mark)
This causes a large proportion of the ultrasound intensity to be reflected. (1 mark)
(b)
States R = [(Z2 − Z1)/(Z2 + Z1)] squared. (1 mark)
Z1 and Z2 are the acoustic impedances of the two media. (1 mark)
(c)
Strong reflection prevents significant transmission beyond the boundary, reducing penetration depth or causing acoustic shadowing. (1 mark)

