OCR Specification focus:
‘External and internal intercostal muscles, the ribcage and the diaphragm coordinate to change thoracic volume and pressure, ventilating the lungs during inspiration and expiration.’
Mammalian ventilation mechanics enable continuous oxygen intake and carbon dioxide removal. Coordinated muscle and pressure changes within the thorax drive efficient inspiration and expiration essential for aerobic respiration.
Structure of the Thoracic Cavity
The thoracic cavity forms the space housing the lungs, protected by the ribcage and separated from the abdominal cavity by the diaphragm. This enclosed space allows pressure changes to drive air movement during ventilation, maintaining the necessary gas exchange gradient between alveoli and blood.
Key Components
Ribcage: Protects lungs and provides structural support for muscle attachment.
Diaphragm: A dome-shaped sheet of muscle separating thorax and abdomen; its contraction changes thoracic volume.
Intercostal muscles: Located between ribs, consisting of external and internal intercostal muscles working antagonistically.
Pleural membranes: Two thin layers with pleural fluid between them reduce friction and ensure lungs move smoothly with the thoracic wall.
The coordination of these structures ensures that pressure within the lungs changes appropriately to draw air in and out efficiently.
Principles of Ventilation
Ventilation refers to the mechanical process of moving air in and out of the lungs to maintain gas exchange. It relies on the principle that air moves from areas of higher pressure to lower pressure. Therefore, changing thoracic volume alters thoracic pressure, causing air to flow.
Ventilation: The process of moving air between the atmosphere and the lungs by mechanical changes in thoracic pressure and volume.
When thoracic volume increases, internal air pressure decreases below atmospheric pressure, causing air to enter (inspiration). When thoracic volume decreases, pressure rises above atmospheric pressure, forcing air out (expiration).
Mechanism of Inspiration
During inspiration (inhalation), several coordinated actions increase the volume of the thoracic cavity, reducing internal pressure relative to atmospheric air.
Process of Inspiration
External intercostal muscles contract, pulling the ribs upwards and outwards.
Diaphragm contracts and flattens, moving downwards to increase thoracic volume.
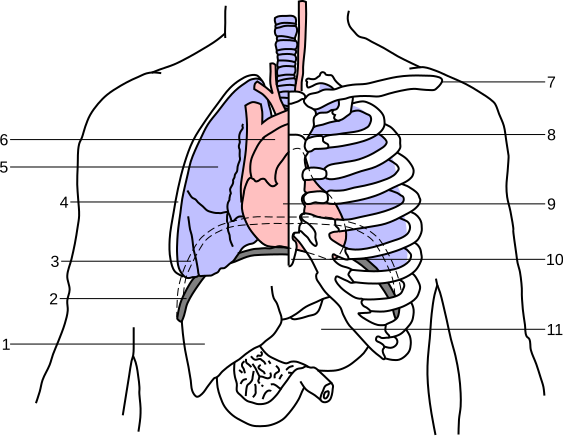
A labelled vector diagram of the diaphragm during inspiration and expiration. It highlights the dome flattening on contraction and the resulting expansion of thoracic volume. The pleural space and adjacent thoracic landmarks are included; these details exceed the syllabus slightly but aid orientation. Source.
Internal intercostal muscles relax to allow rib movement.
Pleural membranes transmit this expansion to the lungs, causing alveoli to expand.
Air pressure inside the lungs falls below atmospheric pressure, so air flows into the lungs.
This negative pressure ventilation ensures efficient air entry without active suction. The expansion of the lungs stretches elastic tissue, storing potential energy for recoil during expiration.
Negative Pressure Ventilation: A breathing mechanism where air enters the lungs because internal air pressure drops below atmospheric pressure.
Mechanism of Expiration
During expiration (exhalation), the process reverses, reducing thoracic volume and increasing internal pressure, forcing air out of the lungs.
Process of Expiration
External intercostal muscles relax, allowing ribs to move downwards and inwards.
Diaphragm relaxes, returning to its dome shape, decreasing thoracic volume.
Elastic fibres in lung tissue recoil, aiding the expulsion of air.
Internal intercostal muscles may contract during forced expiration, pulling ribs further down to increase pressure.
In normal, quiet breathing, expiration is mainly passive, driven by elastic recoil rather than muscle contraction. However, during vigorous breathing (e.g., exercise), expiration becomes active, with additional muscular effort to speed up airflow.
Relationship Between Pressure and Volume
Ventilation operates on the principle of Boyle’s Law, which describes the inverse relationship between pressure and volume in a closed system.
EQUATION
—-----------------------------------------------------------------
Boyle’s Law: P ∝ 1/V
P = Pressure within the lungs (Pa or kPa)
V = Volume of the thoracic cavity (m³ or L)
—-----------------------------------------------------------------
As thoracic volume increases, pressure decreases; as volume decreases, pressure increases. This simple relationship governs airflow during the respiratory cycle.
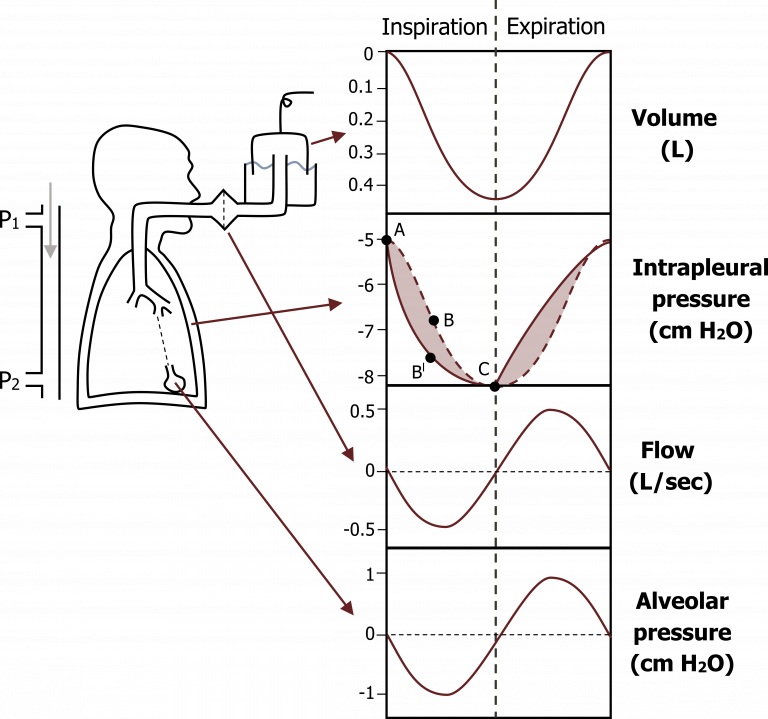
Graphical summary of lung volume, alveolar pressure, intrapleural pressure, and airflow across one respiratory cycle. It illustrates how volume changes create pressure gradients that drive ventilation. Multiple traces are shown; the level of detail slightly exceeds the syllabus but maps exactly to your explanation. Source.
Role of Elastic Fibres and Smooth Muscle
Elastic fibres within alveoli and bronchioles are critical for restoring the lungs to their resting shape after inspiration. This elasticity prevents alveolar collapse while enabling passive exhalation.
Smooth muscle controls the diameter of bronchi and bronchioles, adjusting airflow resistance. During exercise, bronchodilation increases air flow, whereas bronchoconstriction can occur due to allergic reactions or asthma.
Elastic Recoil: The return of lung tissues to their original volume due to elastic fibres after being stretched during inspiration.
Pressure Changes During the Breathing Cycle
The cycle of inspiration and expiration can be visualised through the alternating changes in thoracic volume, alveolar pressure, and airflow.
Inspiration
Thoracic volume: Increases
Alveolar pressure: Falls below atmospheric pressure
Airflow: Into the lungs
Expiration
Thoracic volume: Decreases
Alveolar pressure: Rises above atmospheric pressure
Airflow: Out of the lungs
Maintaining a smooth gradient ensures efficient gas exchange within alveoli, as oxygen continuously diffuses into the bloodstream and carbon dioxide diffuses out.
Control of Ventilation Rate
Although ventilation is largely automatic, it is regulated by the respiratory centre in the medulla oblongata. Chemoreceptors detect carbon dioxide concentration and blood pH, adjusting the rate and depth of breathing accordingly. Increased CO₂ lowers blood pH, stimulating faster, deeper breaths to restore homeostasis.
Homeostasis: The maintenance of stable internal conditions despite external changes.
This regulatory mechanism ensures that ventilation matches metabolic demand, especially during exercise or stress.
Summary of Key Features
Ventilation involves coordinated muscle activity to change thoracic volume and pressure.
Inspiration is active: diaphragm and external intercostals contract.
Expiration is usually passive: muscles relax and elastic recoil occurs.
Forced breathing recruits additional muscles for greater pressure changes.
The pleural membranes and thoracic structure ensure pressure differences efficiently move air in and out of the lungs.
Ventilation maintains the concentration gradients required for effective gas exchange across the alveolar surface.
FAQ
The pleural membranes — the visceral and parietal pleura — form a continuous double layer around each lung with a thin film of pleural fluid between them.
This fluid creates surface tension, allowing the lungs to adhere to the thoracic wall. When the thoracic cavity expands or contracts, the lungs follow passively, ensuring volume and pressure changes are efficiently transmitted.
If the pleural seal is broken (as in a punctured lung), pressure equalises and the lung collapses, a condition known as a pneumothorax.
Expiration at rest is mostly passive because of elastic recoil.
After inspiration, the elastic fibres in lung tissue and the chest wall return to their resting shape.
The diaphragm and external intercostal muscles relax, reducing thoracic volume.
This raises alveolar pressure slightly above atmospheric pressure, pushing air out naturally.
Active expiration only occurs during vigorous exercise or forced breathing, when the internal intercostal and abdominal muscles contract to expel air more quickly.
Posture influences how easily the diaphragm and thoracic wall move.
Upright position: Diaphragm descends more effectively, allowing maximum lung expansion and better ventilation of lower alveoli.
Supine (lying flat): Abdominal organs press upward on the diaphragm, reducing thoracic expansion and tidal volume.
Slumped posture: Compresses the chest cavity, limiting lung expansion and reducing airflow efficiency.
This is why patients with breathing difficulties are often positioned upright to aid ventilation.
Intrapleural pressure is always negative relative to atmospheric pressure, keeping lungs expanded.
During inspiration, thoracic expansion makes intrapleural pressure more negative (further drop).
During expiration, thoracic volume decreases, making the pressure slightly less negative.
This cyclical change ensures the lungs remain inflated but still responsive to muscle-driven volume changes. If intrapleural pressure becomes positive, the lung can detach from the chest wall and collapse.
Exercise increases both rate and depth of ventilation to meet higher oxygen demand.
Inspiration: Accessory muscles (sternocleidomastoid and pectoralis minor) assist the diaphragm and external intercostals to lift the ribs higher and expand the thorax further.
Expiration: Becomes active; internal intercostals and abdominal muscles contract forcefully to expel air rapidly.
Result: Greater tidal volume and more efficient gas exchange.
These changes are coordinated by neural and chemical control centres that monitor rising carbon dioxide levels and blood pH.
Practice Questions
Question 1 (2 marks)
Describe how the diaphragm and external intercostal muscles work together during inspiration in mammals.
Mark scheme:
1 mark: Diaphragm contracts and flattens, increasing the volume of the thoracic cavity.
1 mark: External intercostal muscles contract, pulling the ribs upwards and outwards, further increasing thoracic volume and decreasing pressure to draw air into the lungs.
Question 2 (5 marks)
Explain how changes in thoracic volume and pressure bring about ventilation in mammals during both inspiration and expiration.
Mark scheme:
1 mark: Air moves from areas of high pressure to low pressure.
1 mark: During inspiration, diaphragm contracts and flattens while external intercostal muscles contract, raising the ribcage.
1 mark: These actions increase thoracic volume and decrease thoracic pressure below atmospheric pressure, causing air to flow into the lungs.
1 mark: During expiration, diaphragm relaxes and returns to a dome shape, and external intercostal muscles relax, reducing thoracic volume.
1 mark: The increase in pressure above atmospheric pressure forces air out of the lungs; elastic recoil of lung tissue aids this process.

