OCR Specification focus:
‘Analyse relationships between tidal volume, vital capacity, breathing rate and oxygen uptake, interpreting data from spirometers or data loggers to quantify ventilation changes.’
Understanding lung volumes and spirometry is essential to analysing how the human respiratory system adapts to meet oxygen demands. These measurements provide quantitative insights into ventilation efficiency and respiratory health.
Lung Volumes
The lungs contain several measurable volumes that represent air movement during breathing cycles. Together, these form the basis of understanding pulmonary function.
Tidal Volume (TV)
Tidal Volume: The volume of air inhaled or exhaled in one normal breath, typically about 0.5 dm³ in a healthy adult at rest.
Tidal volume ensures a continuous exchange of oxygen and carbon dioxide even at rest, maintaining the concentration gradients essential for diffusion in the alveoli.
Inspiratory and Expiratory Reserve Volumes
During vigorous breathing, additional air can be moved beyond normal tidal volumes.
Inspiratory Reserve Volume (IRV): Extra air that can be forcibly inhaled after a normal inspiration.
Expiratory Reserve Volume (ERV): Additional air that can be forcibly exhaled after a normal expiration.
These reserve volumes reflect the flexibility of the thoracic cavity and elasticity of lung tissue.
Residual Volume (RV)
Residual Volume: The volume of air remaining in the lungs after a full, forceful exhalation; prevents lung collapse and maintains alveolar inflation.
Residual volume is essential because it keeps alveoli partially inflated, maintaining efficient gas exchange between breaths.
Vital Capacity (VC)
EQUATION
—-----------------------------------------------------------------
Vital Capacity (VC) = Tidal Volume (TV) + Inspiratory Reserve Volume (IRV) + Expiratory Reserve Volume (ERV)
TV = Air per normal breath (dm³)
IRV = Extra inhaled air (dm³)
ERV = Extra exhaled air (dm³)
—-----------------------------------------------------------------
Vital capacity represents the maximum volume of air a person can exchange in one full breath cycle. It varies with age, sex, body size, and physical fitness. Larger lungs or stronger respiratory muscles typically yield higher VC values.
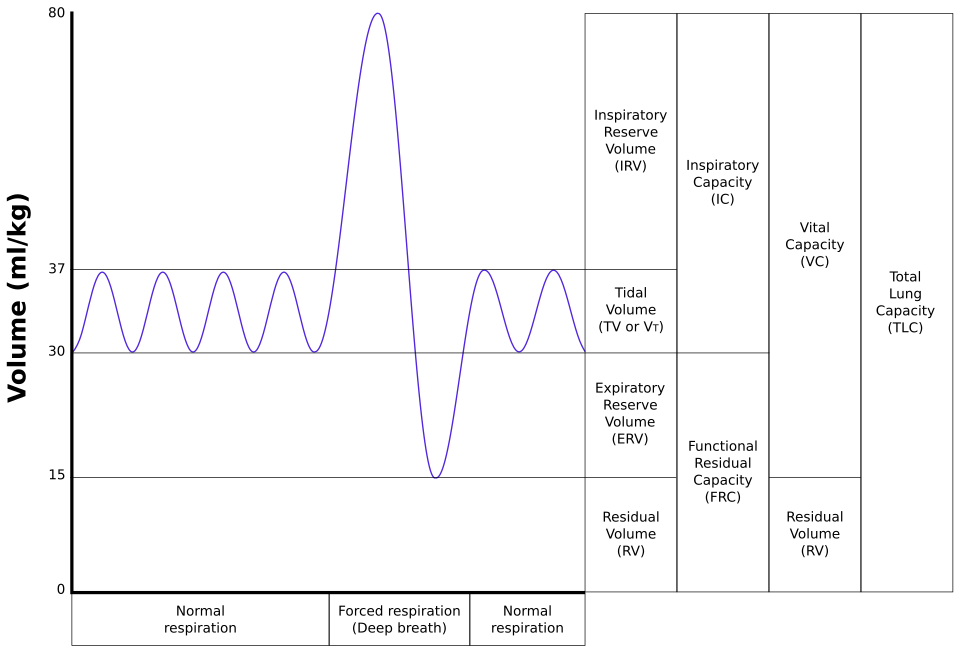
A spirogram illustrating normal tidal breaths followed by maximal inspiration and expiration, with key volumes and capacities labelled (TV, IRV, ERV, RV, VC). This visual supports quantitative analysis of ventilation from spirometry traces. The diagram also labels IC and FRC, which are useful context but go beyond the OCR focus on TV, VC, breathing rate and oxygen uptake. Source.
Total Lung Capacity (TLC)
Total Lung Capacity combines all air volumes the lungs can contain.
EQUATION
—-----------------------------------------------------------------
Total Lung Capacity (TLC) = Vital Capacity (VC) + Residual Volume (RV)
VC = Maximum air exchanged
RV = Air remaining post-exhalation
—-----------------------------------------------------------------
This measure reflects the complete capacity of the respiratory system, crucial for comparing lung performance across individuals or in medical diagnostics.
Spirometry and Ventilation Measurement
The Spirometer
A spirometer is an instrument used to measure lung volumes and airflow during breathing. Traditional water-bell spirometers record air displacement on a kymograph, while modern digital spirometers use sensors connected to data loggers for real-time recording.
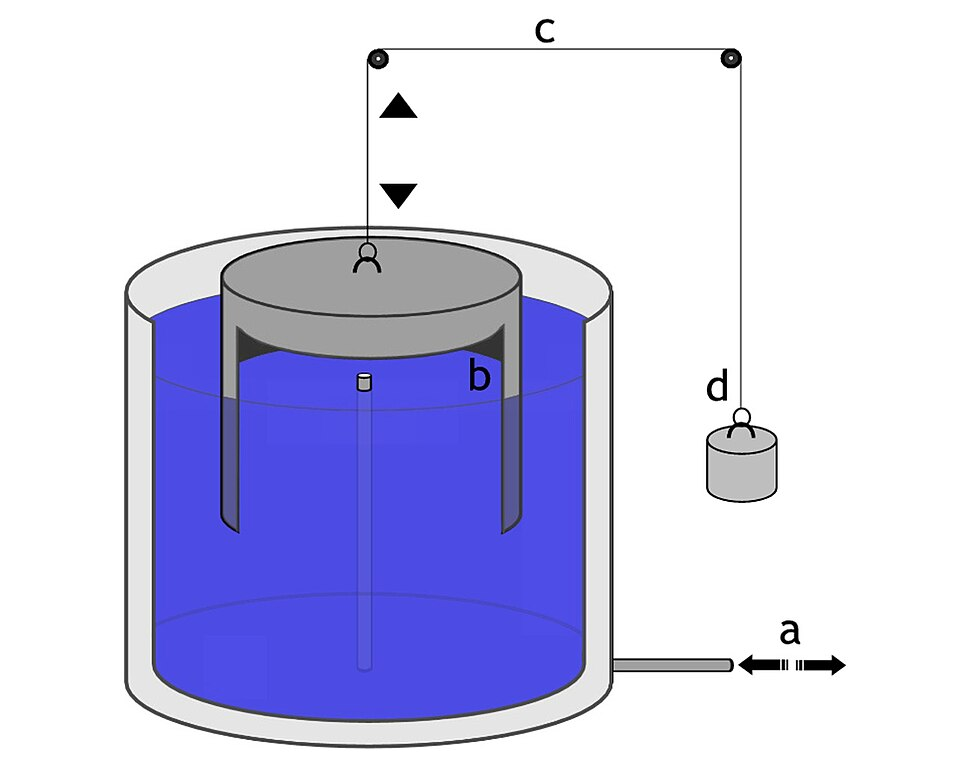
Diagram of a water-seal spirometer, in which breathing moves an inverted bell through water to record volume changes. This setup underlies classic spirometer traces used to derive TV, IRV, ERV, RV and VC. Labels are in German, but the components (bell, water reservoir, pulleys) are schematic and directly map to the apparatus described. Source.
The spirometer trace records:
Upward deflection: inspiration (air drawn into the lungs)
Downward deflection: expiration (air expelled)
Amplitude: tidal volume and other parameters
Spirometry allows analysis of both resting ventilation and responses to exercise, providing insights into respiratory efficiency.
Key Measurable Parameters
Tidal Volume (TV) – height of small waves on trace
Vital Capacity (VC) – difference between deepest inspiration and full expiration
Breathing Rate (f) – number of breaths per minute
Oxygen Uptake Rate – rate at which oxygen is consumed from inhaled air
Oxygen uptake can be inferred from the rate of CO₂ production or by using oxygen sensors in modern spirometric setups.
Ventilation and Oxygen Uptake
Ventilation rate quantifies the volume of air entering and leaving the lungs per minute. It reflects both frequency and depth of breathing.
EQUATION
—-----------------------------------------------------------------
Ventilation Rate (VE) = Tidal Volume (TV) × Breathing Rate (f)
VE = Total air ventilated per minute (dm³ min⁻¹)
TV = Volume per breath (dm³)
f = Breaths per minute
—-----------------------------------------------------------------
This equation demonstrates how both breathing rate and tidal volume adapt to meet metabolic demands. For example:
During rest: low TV and moderate f
During exercise: both increase to supply additional oxygen and remove carbon dioxide
Oxygen Uptake
Oxygen Uptake: The rate at which oxygen is absorbed from alveolar air into the bloodstream, often expressed in cm³ O₂ per minute.
Oxygen uptake depends on:
The steepness of diffusion gradients between alveoli and capillaries
Haemoglobin concentration and affinity
Cardiac output, which transports oxygen to tissues
Spirometric data, or readings from data loggers, allow calculation of oxygen uptake by measuring the decrease in gas volume due to oxygen consumption.

Photograph of a digital spirometry sensor used with data-logging systems to capture volume-time traces for analysis of TV, VC, breathing rate and oxygen uptake. This real-world device exemplifies the modern alternative to water-bell spirometers described in the notes. The image does not add extra physiological content beyond the syllabus focus. Source.
Factors Affecting Lung Volumes and Ventilation
Physiological Factors
Age: Elasticity of lung tissue decreases, reducing VC and TLC.
Sex: Males typically exhibit larger lung volumes due to greater thoracic dimensions.
Body size: Larger body frames correlate with greater lung capacity.
Physical fitness: Training increases respiratory muscle strength and VC.
Environmental and Medical Factors
Altitude: Lower oxygen partial pressure stimulates increased ventilation rate.
Smoking: Damages alveoli and reduces elastic recoil, lowering VC.
Respiratory diseases:
Asthma narrows airways, reducing airflow.
Emphysema destroys alveolar walls, decreasing surface area.
Fibrosis increases diffusion distance and reduces elasticity.
These factors influence spirometry traces, allowing clinicians to identify obstructive or restrictive lung disorders.
Analysing Spirometer Traces
Students must interpret spirometer data to quantify ventilation changes and identify relationships between variables. Key interpretations include:
Increased tidal volume and breathing rate during exercise indicate greater oxygen demand.
Reduced vital capacity may suggest lung disease or restricted thoracic expansion.
Changes in oxygen uptake rate show how efficiently the respiratory system adapts to metabolic activity.
By analysing these relationships, spirometry provides a quantitative understanding of ventilation mechanics, respiratory adaptation, and overall lung function, fulfilling the OCR requirement to relate and interpret tidal volume, vital capacity, breathing rate, and oxygen uptake.
FAQ
A spirometer includes a carbon dioxide absorber, such as soda lime or potassium hydroxide, which removes CO₂ from exhaled air.
As the subject breathes, only oxygen is removed from the chamber for respiration, causing the total gas volume to fall. By measuring this decrease over time, oxygen uptake can be calculated.
This setup ensures that changes in gas volume represent oxygen consumption alone, not the combined effects of oxygen use and carbon dioxide release.
A nose clip prevents air from entering or leaving through the nasal passages, ensuring all ventilation occurs through the mouthpiece connected to the spirometer.
This makes the volume and flow readings accurate and consistent. Without a nose clip, exhaled air could escape via the nose, leading to underestimation of tidal volume and oxygen uptake.
It also standardises conditions between participants, improving the reliability of comparative data.
Key safety steps include:
Using a sterilised or disposable mouthpiece to prevent cross-contamination.
Ensuring the soda lime absorber is securely placed to avoid inhalation of chemicals.
Filling the chamber with fresh air and checking oxygen concentration before each use.
Allowing the subject to rest between trials to prevent dizziness or hyperventilation.
Spirometers should also be regularly checked for leaks to maintain valid readings.
Variation arises from several physiological and environmental factors:
Fitness level: trained individuals have stronger respiratory muscles and higher vital capacities.
Smoking history: reduces elasticity and functional alveolar surface area.
Altitude of residence: people living at high altitudes often develop larger lung capacities over time.
Even posture, genetics, and thoracic cavity size can influence overall vital capacity and total lung capacity.
Regular aerobic exercise leads to measurable adaptations that improve ventilatory efficiency:
Increased vital capacity due to stronger diaphragm and intercostal muscles.
Lower resting breathing rate, as more oxygen is exchanged per breath.
Higher oxygen uptake rate during exercise, shown by steeper spirometer trace gradients.
These adaptations enhance gas exchange efficiency, meaning athletes can maintain higher oxygen delivery with less respiratory effort.
Practice Questions
Question 1 (2 marks)
Define tidal volume and vital capacity, and explain how they differ in the context of ventilation.
Mark scheme:
1 mark for correctly defining tidal volume: volume of air inhaled or exhaled in a normal breath (about 0.5 dm³ in a healthy adult).
1 mark for correctly defining vital capacity and describing the difference: maximum volume of air that can be exchanged in one full breath cycle (sum of tidal volume, inspiratory reserve volume, and expiratory reserve volume).
Question 2 (5 marks)
A spirometer was used to measure a student’s breathing before and after exercise. Explain how and why both tidal volume and breathing rate change during exercise, and describe how oxygen uptake can be measured using a spirometer.
Mark scheme:
1 mark for stating that tidal volume increases during exercise to bring more air into the lungs per breath.
1 mark for stating that breathing rate increases to raise overall ventilation rate and meet higher oxygen demand.
1 mark for explaining that increased ventilation maintains a steep diffusion gradient for oxygen and carbon dioxide between alveoli and blood.
1 mark for describing how oxygen uptake can be measured: by recording the reduction in gas volume in the spirometer as oxygen is consumed.
1 mark for stating that carbon dioxide is absorbed (e.g. by soda lime), allowing oxygen uptake to be determined accurately from the decrease in total gas volume.

