OCR Specification focus:
‘Kidney failure affects glomerular filtration rate and electrolyte balance; treatments include haemodialysis and kidney transplants.’
Kidney failure occurs when the kidneys can no longer efficiently filter waste, regulate electrolytes, or control fluid balance, requiring medical intervention through dialysis or transplantation.
Understanding Kidney Failure
The Role of the Kidneys
The kidneys are essential organs responsible for excretion, osmoregulation, and homeostatic balance. They maintain blood composition by filtering waste, reabsorbing useful substances, and regulating ions and water.
When the kidneys fail, these functions deteriorate, leading to the accumulation of toxic substances and disruption of internal equilibrium.
Causes of Kidney Failure
Kidney failure, or renal failure, may develop acutely or chronically:
Acute kidney injury (AKI): sudden loss of renal function, often due to low blood pressure, infection, or nephrotoxic drugs.
Chronic kidney disease (CKD): gradual, irreversible damage caused by long-term conditions such as diabetes mellitus, hypertension, or autoimmune disorders.
Both forms result in reduced glomerular filtration rate (GFR) and impaired removal of metabolic wastes.
Measuring Kidney Function
Glomerular Filtration Rate (GFR): The rate at which blood is filtered through the glomeruli per minute, used to assess kidney function.
Normal GFR values are typically around 90–120 cm³ min⁻¹, depending on age and health. A decline in GFR is a key indicator of kidney failure. When GFR falls below 15 cm³ min⁻¹, renal replacement therapy becomes necessary.
Consequences of Kidney Failure
Kidney failure has widespread effects on the body due to the accumulation of metabolic waste and loss of homeostatic control:
Uraemia: build-up of urea and other toxins leading to fatigue, nausea, and confusion.
Electrolyte imbalance: particularly hyperkalaemia (excess potassium) which can cause dangerous cardiac arrhythmias.
Oedema: fluid retention in tissues due to poor osmoregulation.
Anaemia: reduced erythropoietin secretion leads to decreased red blood cell production.
Acidosis: inability to excrete hydrogen ions, lowering blood pH.
Without treatment, kidney failure is fatal due to toxin accumulation and fluid imbalance.
Treatment Options for Kidney Failure
1. Dialysis
Dialysis is a method for artificially removing waste products and excess fluid from the blood. It substitutes for some kidney functions but does not cure the condition.
There are two main types of dialysis: haemodialysis and peritoneal dialysis.
Haemodialysis
Haemodialysis is performed using a dialysis machine and a semipermeable membrane. Blood is withdrawn from the patient, filtered, and returned to the body.
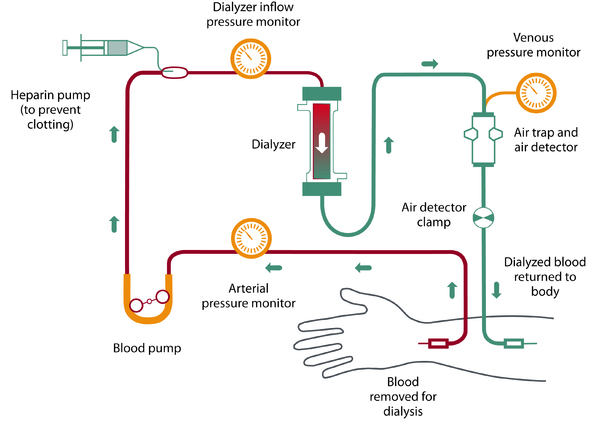
A labelled schematic of the haemodialysis circuit showing blood withdrawal, pumping, anticoagulation, passage through the dialyser, and monitored return to the patient. The diagram highlights counter-current flow and safety features such as pressure monitoring and air detection. This includes device components beyond the syllabus (e.g., specific monitors) to clarify how safe filtration is maintained. Source.
Process Overview:
Blood flows from an artery into the dialysis machine.
The dialysis fluid (dialysate) has a composition similar to blood plasma but without waste products.
Waste substances such as urea, creatinine, and excess ions diffuse across the membrane into the dialysate by diffusion and osmosis.
The cleaned blood returns to the patient via a vein.
Key Features:
Countercurrent flow between blood and dialysate maintains a steep concentration gradient for efficient diffusion.
The dialysate composition prevents loss of useful substances like glucose and amino acids.
Bicarbonate ions in the fluid help correct blood pH.
Patients typically undergo haemodialysis three times per week, each session lasting several hours.
Peritoneal Dialysis
Peritoneal dialysis uses the patient’s own peritoneum (lining of the abdominal cavity) as the dialysis membrane.
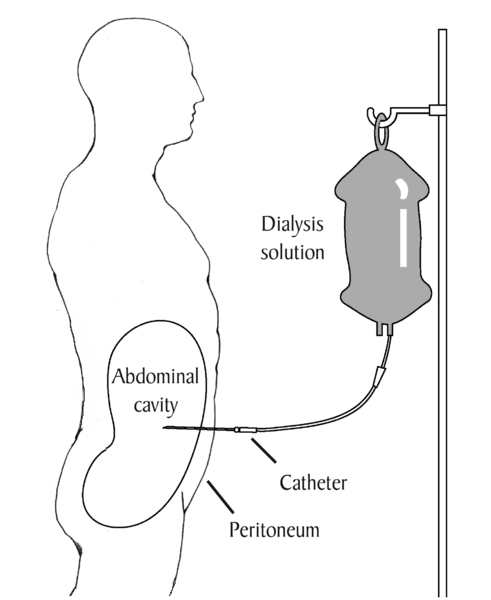
A labelled diagram of continuous ambulatory peritoneal dialysis (CAPD), showing dialysate inflow via a permanent catheter into the peritoneal cavity. Gas-exchange style diffusion across the peritoneal membrane enables removal of urea, creatinine, and excess ions. The diagram is focused and includes only essential labels aligned to the syllabus. Source.
Process Overview:
Dialysis fluid is introduced into the peritoneal cavity via a catheter.
Diffusion of waste products and ions occurs between the blood in capillaries of the peritoneal membrane and the dialysis fluid.
After several hours, the fluid containing wastes is drained and replaced.
Advantages and Disadvantages:
Can be performed at home and offers greater flexibility.
Less efficient than haemodialysis and carries risk of peritonitis (infection of the peritoneal membrane).
Comparing Dialysis Methods
Haemodialysis provides rapid clearance of toxins but is time-consuming and requires hospital visits. Peritoneal dialysis is slower but continuous, allowing a more stable internal environment.
Both methods demand strict dietary control, particularly of protein, salt, and fluid intake, to prevent accumulation of waste and swelling between treatments.
2. Kidney Transplant
A kidney transplant offers a long-term solution by replacing the damaged kidney with a healthy one from a donor.
Procedure:
The new kidney is surgically placed in the lower abdomen and connected to the patient’s renal artery, renal vein, and ureter.
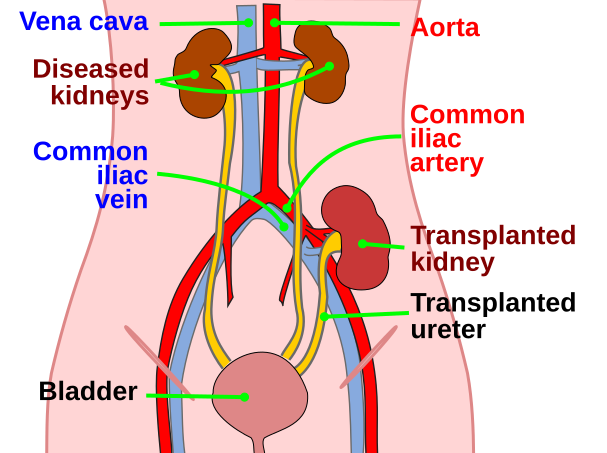
Diagram showing the anatomical position of a transplanted kidney in the lower abdomen (iliac fossa) with the ureter leading to the bladder. This directly supports the description of transplant placement in your notes. Labels are minimal and focused on location; surgical anastomoses are implied rather than fully detailed. Source.
The recipient’s non-functioning kidneys are usually left in place unless they cause infection or hypertension.
Donor Sources:
Living donors (usually relatives with tissue compatibility).
Deceased donors (organ retrieved soon after death).
Advantages:
Restores nearly full kidney function.
Eliminates need for dialysis.
Improves quality of life and long-term survival rate.
Disadvantages:
Requires immunosuppressant drugs to prevent rejection, increasing infection risk.
Limited availability of suitable donors.
Risk of graft rejection or transplant failure over time.
Graft Rejection and Immunosuppression
Graft Rejection: The immune response of the recipient’s body recognising the donor kidney as foreign and attacking it.
To minimise rejection, tissue typing ensures donor and recipient have similar human leukocyte antigens (HLA). Post-transplant, patients must take immunosuppressive medication such as ciclosporin or tacrolimus for life.
Although these drugs prevent rejection, they weaken the immune system, making patients more vulnerable to infections and some cancers.
Evaluating Treatment Approaches
The choice between dialysis and transplant depends on several factors:
Age and general health of the patient.
Availability of donor organs.
Suitability for surgery.
Personal preference and lifestyle.
Economic and healthcare considerations.
In the UK, dialysis often serves as a short-term measure while awaiting transplantation, though some patients remain on dialysis long-term if transplant is not feasible.
Monitoring and Long-Term Management
After treatment, patients require regular monitoring of:
GFR and electrolyte balance.
Blood pressure and hydration status.
Signs of infection or rejection.
Lifestyle adaptations such as balanced diet, limited alcohol, and smoking cessation further enhance long-term health outcomes.
FAQ
Dialysis begins when kidney function falls below a critical threshold, typically when the glomerular filtration rate (GFR) drops below 15 cm³ min⁻¹.
Symptoms such as persistent nausea, oedema, fatigue, or dangerously high potassium levels also trigger the need for intervention.
Other considerations include:
The rate of decline in kidney function.
The patient’s overall health and tolerance to waste accumulation.
The presence of fluid overload or uraemic complications such as pericarditis.
Doctors balance timing carefully—starting too early increases dependency on dialysis, while starting too late risks serious metabolic imbalance.
Haemodialysis removes waste and water only during treatment sessions, not continuously. Excessive protein intake produces more urea, increasing toxin load between sessions.
Salt causes water retention and raises blood pressure, while too much fluid leads to swelling and strain on the heart.
Dietary control helps maintain:
Stable blood pressure.
Appropriate blood electrolyte balance.
Comfortable fluid levels between dialysis sessions.
Patients work with dietitians to balance nutrition while minimising metabolic waste accumulation.
Both forms use the peritoneum as the dialysis membrane but differ in how fluid exchanges occur.
CAPD: The patient manually drains and refills dialysis fluid 3–5 times a day. Exchanges occur using gravity, allowing treatment flexibility.
APD: A machine (cycler) automatically performs exchanges overnight while the patient sleeps.
APD is often preferred for younger or working patients as it provides daytime freedom, while CAPD offers simplicity and independence without machinery. Both achieve similar waste removal if performed correctly.
Immunosuppressants prevent the immune system from recognising the donor kidney as foreign and attacking it. Drugs such as ciclosporin or tacrolimus inhibit T-lymphocyte activation, preventing graft rejection.
However, suppression of the immune response increases susceptibility to:
Infections, including viral and fungal.
Certain cancers, due to reduced immune surveillance.
Drug toxicity, particularly to the liver and kidneys themselves.
Balancing effectiveness and safety requires regular monitoring and dose adjustment throughout the patient’s life.
Compatibility is assessed through:
Blood group (ABO) matching to prevent immediate rejection.
Human leukocyte antigen (HLA) typing, comparing six key antigens inherited from parents; more matches mean lower rejection risk.
Crossmatching, mixing donor and recipient blood samples to detect antibody reactions.
If no reaction occurs, the transplant is more likely to succeed.
In some cases, paired or pooled donation schemes allow incompatible pairs to swap donors with other pairs, improving match rates and outcomes.
Practice Questions
Question 1 (2 marks)
Explain why patients with kidney failure may experience swelling in their ankles and feet.
Mark scheme:
1 mark for stating that kidney failure leads to impaired removal of excess water from the blood.
1 mark for explaining that this results in fluid accumulation (oedema) in tissues, particularly in the lower limbs due to gravity.
Question 2 (5 marks)
Compare and contrast haemodialysis and peritoneal dialysis as treatments for kidney failure. In your answer, refer to how each method removes waste products and maintains homeostasis.
Mark scheme:
1 mark for describing that haemodialysis uses a machine with a semipermeable membrane to filter blood externally.
1 mark for describing that peritoneal dialysis uses the patient’s own peritoneum as the dialysis membrane.
1 mark for explaining that in both methods, waste products and excess ions move by diffusion from blood to dialysis fluid.
1 mark for noting that haemodialysis is intermittent (typically 3 times a week) whereas peritoneal dialysis is continuous (e.g., CAPD).
1 mark for comparing advantages/disadvantages such as haemodialysis requiring hospital visits but being more efficient, while peritoneal dialysis allows home treatment but carries a risk of infection (peritonitis).

