OCR Specification focus:
‘Discuss PET applications in diagnosis and considerations when deploying expensive scanners.’
Positron emission tomography (PET) provides functional medical imaging that reveals metabolic activity inside the body, supporting diagnosis of cancers, neurological disorders, and cardiovascular disease with high sensitivity and detail.
Understanding PET in Diagnostic Medicine
PET is a form of nuclear medical imaging that detects gamma photons produced when a positron-emitting radionuclide undergoes annihilation inside the body. Unlike structural imaging techniques such as CT or X-ray radiography, PET provides functional, physiological, and metabolic information. This makes it especially valuable for identifying abnormal biological processes before they manifest as anatomical changes.
The Diagnostic Role of PET
PET is fundamentally used to identify areas of abnormally high or low metabolic activity, which often correspond to disease. Because many pathological processes involve altered glucose consumption, oxygen use, or blood flow, PET imaging is particularly effective for early detection.
Core Diagnostic Applications
PET serves several major diagnostic areas:
Oncology
PET is widely used to detect malignant tumours, determine cancer staging, assess treatment effectiveness, and evaluate recurrence. Many cancers show increased uptake of radiotracers due to enhanced metabolic rates.Neurology
PET assists in diagnosing degenerative diseases such as Parkinson’s and Alzheimer’s by mapping regions of reduced neuronal activity or altered neurotransmitter distribution.Cardiology
PET can identify areas of poor perfusion or damaged myocardial tissue, providing information about coronary artery disease or cardiac viability.
Between these applications, PET helps clinicians detect disease at very early stages.
Radiotracers and Biological Insight
A key advantage of PET lies in the versatility of its radiotracers, substances tagged with positron-emitting isotopes. After administration, radiotracers accumulate in tissues according to specific biochemical pathways, enabling the scan to highlight functional processes.
Commonly Used PET Radiotracers
Fluorodeoxyglucose (FDG) — a glucose analogue used to assess metabolic activity
Oxygen-15 and Carbon-11 compounds — monitor blood flow and biochemical reactions
Ammonia-13 — used in cardiac perfusion studies
Each tracer targets a different physiological process, making PET highly adaptable.
Radioactive Decay and Annihilation
When a radiotracer decays, it emits a positron, the antiparticle of the electron. After travelling a short distance, the positron encounters an electron, resulting in annihilation and the release of two gamma photons.
Positron–electron annihilation: The process in which a positron and an electron collide and convert their mass into two gamma photons emitted in opposite directions.
These photons are detected by the PET scanner, allowing the system to reconstruct the precise location of the decay.
A normal sentence must follow definition blocks to maintain appropriate separation within the notes. Because of annihilation physics, PET offers extremely sensitive detection of functional changes.
Image Formation and Diagnostic Interpretation
PET scanners rely on precise detection of coincident gamma photons.
Coincidence Detection
The scanner contains a circular array of scintillation detectors that register gamma photons. When two photons are detected simultaneously on opposite sides of the ring, the system identifies a line of response along which the annihilation occurred.
This enables the computer software to map many thousands of these events and generate a detailed image of tracer concentration throughout the body.
Interpreting PET Images
Clinicians assess PET images by examining:
Regions of unexpectedly high tracer uptake (often called ‘hot spots’)
Regions of reduced uptake (‘cold spots’)
Symmetry across paired organs
Changes relative to earlier scans
These patterns form the basis of diagnostic reasoning.
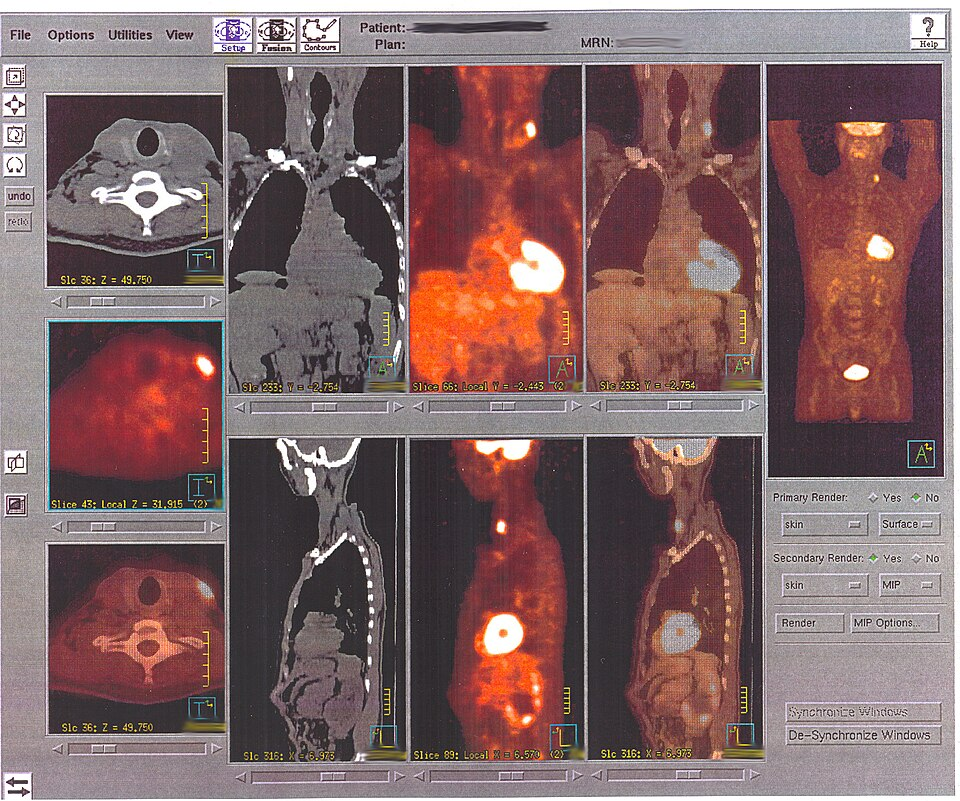
Whole-body PET image showing multiple foci of increased tracer uptake corresponding to metastatic lymph-node disease. Areas of intense activity appear as bright “hot spots”, illustrating how PET reveals abnormal metabolic activity before structural changes are obvious. The image includes pathological detail beyond the OCR specification but is used solely to exemplify diagnostic interpretation of uptake patterns. Source.
Why PET Is Valuable for Diagnosis
PET is particularly useful because:
It detects functional abnormalities before structural changes occur.
It supports treatment planning, showing how far a condition has progressed.
It reveals how tissues respond to therapy over time.
It identifies tumours and metastases that may be invisible on anatomical scans.
The ability to track dynamic processes such as glucose uptake or blood flow makes PET one of the most informative imaging techniques available to clinicians.
Limitations and Considerations When Deploying PET Scanners
Although PET offers exceptional diagnostic capability, its use involves important considerations, especially because scanners are expensive and complex to operate.

Photograph of a modern PET/CT scanner in a hospital imaging suite, with a patient positioned on the moving couch inside the gantry. The system combines PET detectors with an integrated CT unit, reflecting the hybrid scanners commonly used for clinical diagnosis and treatment planning. The image shows additional room details not required by the OCR specification but simply provides context for where PET diagnosis takes place. Source.
Financial and Logistical Considerations
High purchase and maintenance costs make PET scanners a major investment for hospitals.
PET requires access to a cyclotron or distribution network capable of producing short-lived isotopes.
Facilities need strict radiation-safety infrastructure, shielding, and staff training.
These factors influence decisions about where PET scanners can be installed.
Patient and Clinical Considerations
Because tracers emit radiation, PET requires careful dose management, though doses are generally low.
Patients must remain still for accurate imaging, which can be challenging for some individuals.
Clinicians must evaluate PET findings in context with other investigations to avoid misinterpretation.
A normal sentence ensures conceptual clarity between detailed sections and supports coherence in the learning material.
Weighing Benefits Against Costs
Despite its expense, PET often reduces the need for exploratory surgery, detects disease earlier, and streamlines treatment, making it cost-effective in many clinical pathways. Hospitals must balance these advantages against financial and operational constraints when deciding to introduce PET technology.
FAQ
PET tracers are designed to mimic specific biological molecules, so each one highlights a distinct physiological process. For example, fluorodeoxyglucose behaves like glucose and therefore maps metabolic rate, while oxygen-15 compounds track blood flow or oxygen usage.
Different tracers also vary in half-life and chemical behaviour, which determines whether they are suitable for brain studies, cardiac imaging, or detecting tumours with unusual metabolism.
The positron travels a short distance before annihilation, meaning the place where gamma photons originate is not exactly where the positron was emitted.
Additional limitations come from:
Detector size and arrangement
Timing resolution of coincidence electronics
Scattering of gamma photons in tissue
These combine to produce images that are very sensitive to function but less sharp than structural scans.
PET shows function while CT shows structure, so combining them provides both metabolic and anatomical detail in a single scan.
The CT component also performs attenuation correction, allowing more accurate calculation of tracer concentration and improving the reliability of diagnostic measurements.
Interpretation relies on recognising typical physiological patterns such as high uptake in the brain, heart, kidneys, and bladder.
Clinicians compare:
Symmetry across paired organs
Intensity relative to expected physiological levels
Changes from previous scans
Uptake patterns inconsistent with known anatomy or function
Abnormal regions usually stand out as unexpected or asymmetrical “hot spots”.
Patients receive a low radiation dose from the tracer, so measures focus on minimising unnecessary exposure.
Precautions may include:
Advising patients to hydrate to accelerate tracer clearance
Limiting time spent near vulnerable individuals (pregnant people, infants) for several hours after the scan
Screening for contraindications such as pregnancy or inability to remain still
Facilities also maintain strict control of radioactive materials and follow regulated disposal procedures.
Practice Questions
Question 1 (2 marks)
State two reasons why PET is useful for diagnosing cancer at early stages.
Question 1 (2 marks)
Award 1 mark for each correct point, up to 2 marks.
Detects abnormal metabolic activity before structural changes occur. (1)
Highlights areas of increased glucose uptake typical of malignant tumours. (1)
Allows early identification of metastases not visible on anatomical scans. (1)
Provides high sensitivity to changes in tissue function. (1)
Question 2 (5 marks)
Explain how PET imaging produces a functional map of tracer concentration inside the body. Your answer should refer to the underlying physical processes and how the signals are interpreted by the scanner.
Question 2 (5 marks)
Award marks for the following valid points, up to 5 marks.
Positron-emitting radiotracer is injected and accumulates according to metabolic activity. (1)
Positrons annihilate with electrons, producing two gamma photons. (1)
Gamma photons are emitted in opposite directions at 180 degrees. (1)
Detector ring identifies photon pairs using coincidence detection to define a line of response. (1)
Computer reconstructs many lines of response to generate a functional image showing tracer concentration. (1)

