OCR Specification focus:
‘Skin, blood clotting, wound repair, inflammation, expulsive reflexes and mucous membranes act as non-specific barriers; detailed clotting cascade and skin structure are not required.’
Primary non-specific animal defences form the body’s immediate, general protection against pathogens, providing physical and chemical barriers and rapid immune responses before specific immunity becomes active.
Primary Non-Specific Animal Defences
Non-specific defences are the first line of protection that prevent the entry or spread of pathogens. Unlike specific immune responses, they do not target a particular microorganism but act broadly and immediately. These mechanisms include physical barriers, chemical secretions, and physiological responses that help maintain health by blocking or eliminating potential invaders.
The Skin: A Physical and Chemical Barrier
The skin forms the body’s main external defence. It acts as a tough physical barrier composed of dead, keratinised cells in the epidermis, which prevents pathogen entry. The keratin protein provides mechanical strength and waterproofing.
Beneath the epidermis lies the dermis, which contains connective tissue, capillaries, and sensory receptors. When unbroken, the skin forms an almost impenetrable barrier to most pathogens.
Additionally, the skin secretes sebum, an oily substance produced by sebaceous glands, which maintains a slightly acidic pH. This environment inhibits bacterial growth, adding a chemical layer of defence.
Blood Clotting and Wound Repair
If the skin barrier is breached, blood clotting quickly seals the wound to minimise pathogen entry and fluid loss.
Platelets, which are fragments of larger cells called megakaryocytes, are central to this process. When a blood vessel is damaged, platelets contact exposed collagen fibres, triggering their activation.
Activated platelets release substances such as thromboplastin and serotonin:
Thromboplastin initiates a cascade leading to fibrin formation, which traps red blood cells to form a clot.
Serotonin causes vasoconstriction, narrowing blood vessels to reduce blood flow and aid clot stability.
Once the clot dries, it forms a scab, providing a temporary barrier. Underneath, epidermal cells divide and migrate to close the wound, and fibrous collagen tissue strengthens the repair.
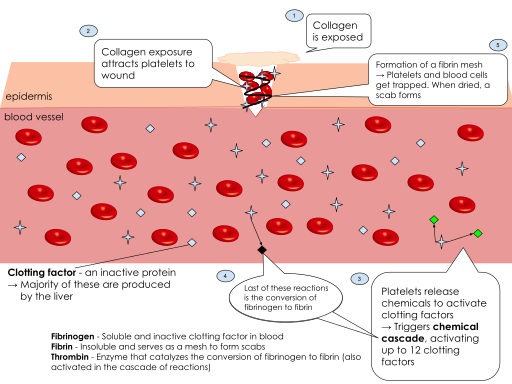
Labeled pathway of blood clot formation, highlighting platelet activation, fibrin generation, and scab formation that seals a breach in the skin barrier. This supports the syllabus focus on blood clotting and wound repair as non-specific defences. The colour-coded clotting factors shown are additional detail not required by OCR. Source.
Blood Clot: A mesh of fibrin fibres and trapped cells that seals a wound and prevents pathogen entry.
This rapid response is essential to prevent infection, particularly in areas prone to injury or microbial exposure.
Inflammation
Inflammation is a vital non-specific defence response to infection, injury, or irritation. It is coordinated by mast cells, which release histamine and other signalling molecules.
Histamine has several effects:
Causes vasodilation, increasing blood flow to the infected area, resulting in redness and warmth.
Increases capillary permeability, allowing plasma, white blood cells, and antibodies to enter tissues.
Promotes the accumulation of phagocytes that engulf pathogens and damaged cells.
These actions produce classic signs of inflammation: pain, heat, redness, and swelling.
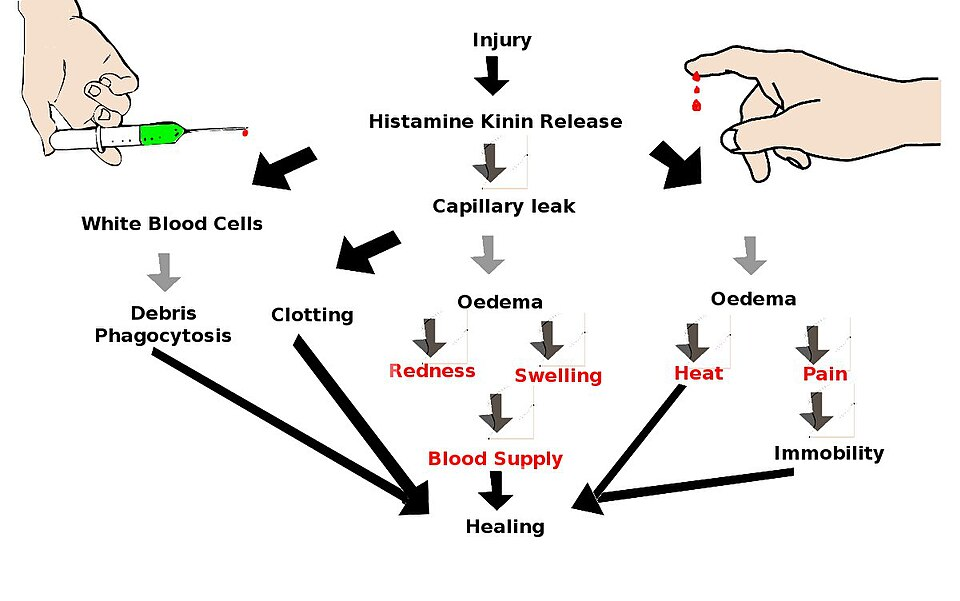
Diagram of the acute inflammatory response showing vasodilation, increased capillary permeability, and leukocyte recruitment that together produce redness, heat, swelling, and pain. This visual consolidates the functional sequence triggered by mast-cell histamine release. No extra mechanistic detail beyond syllabus expectations is included. Source.
Although uncomfortable, inflammation is beneficial as it helps isolate pathogens, facilitates tissue repair, and stimulates immune activation.
Inflammation: A localised tissue response to damage or infection characterised by redness, heat, swelling, and pain.
Inflammation also attracts cytokines, which are cell signalling molecules that coordinate further immune responses.
Mucous Membranes
While the skin covers most of the body, some surfaces must remain moist for function, such as those in the respiratory, digestive, and urogenital tracts. These are lined with mucous membranes, which provide both physical and chemical protection.
Mucus, secreted by goblet cells, traps microorganisms and dust. The mucus layer acts as a sticky barrier, preventing pathogens from reaching underlying tissues.
In the respiratory tract, the mucus is moved by ciliated epithelial cells. Their coordinated, wave-like beating directs mucus towards the throat, where it is swallowed and destroyed by stomach acid.
Mucous Membrane: A moist tissue lining body cavities exposed to the external environment, secreting mucus to trap and remove pathogens.
Other mucosal surfaces, such as those in the eyes, are protected by tears containing lysozyme, an enzyme that breaks down bacterial cell walls. Similarly, saliva and nasal secretions contain lysozyme, enhancing protection in entry points for pathogens.
Expulsive Reflexes
The body also employs expulsive reflexes—automatic physical reactions that remove irritants and pathogens rapidly.
Examples include:
Coughing – clears the respiratory tract of mucus and foreign particles.
Sneezing – expels irritants from nasal passages.
Vomiting – removes harmful substances from the digestive tract.
These reflexes are involuntary and triggered when sensory receptors detect the presence of pathogens or irritants, helping prevent colonisation and infection.
Expulsive Reflex: An automatic muscular response that removes pathogens or irritants from the respiratory or digestive tract.
Though simple, these mechanisms are highly effective when combined with other barriers.
Additional Non-Specific Barriers and Secretions
Beyond the major defences, several chemical secretions contribute to the body’s protective network:
Stomach acid (hydrochloric acid) destroys most ingested pathogens.
Urine flow physically flushes bacteria from the urinary tract.
Earwax provides a physical barrier and traps dust or microbes.
Commensal microorganisms on the skin and in the gut outcompete pathogenic species, forming part of the natural flora.
These defences work synergistically, ensuring that even before specific immunity begins, the body maintains a formidable shield against infection.
Coordination of Non-Specific Responses
Non-specific defences are not isolated systems. They communicate through chemical messengers and cellular signalling, ensuring an integrated response. For example:
Cytokines released during inflammation attract phagocytes, which perform phagocytosis, bridging the transition to specific immunity.
Complement proteins in the blood assist by opsonising pathogens and promoting their destruction.
Although these defences lack memory, they are essential in buying time for the body’s specific immune system to develop targeted responses.
FAQ
The skin is home to diverse populations of commensal microorganisms that form the skin microbiome. These beneficial microbes compete with pathogens for space and nutrients, preventing their colonisation.
Some commensal bacteria also secrete substances like bacteriocins that inhibit pathogen growth or stimulate mild immune responses, keeping the skin’s defences active.
Maintaining a healthy microbiome through good hygiene and minimal overuse of antibacterial products supports this first layer of defence.
Pain during inflammation is primarily due to increased tissue pressure from fluid accumulation and the release of chemical mediators like prostaglandins and bradykinin, which stimulate nerve endings.
Although uncomfortable, pain serves a protective function by reducing movement of the affected area, allowing time for healing.
It also acts as a warning signal that draws attention to infection or injury, encouraging behaviours that prevent further damage.
Both tears and saliva contain lysozyme, an enzyme that hydrolyses bonds in the peptidoglycan cell walls of bacteria, causing lysis and death.
They also contain antibodies (mainly IgA) and salts that inhibit microbial growth.
In addition, the constant flow of these fluids physically washes away microbes from the eye and mouth, reducing the likelihood of infection.
Acute inflammation is short-term, lasting hours to days, and occurs immediately after injury or infection. It involves vasodilation, fluid leakage, and the recruitment of neutrophils.
Chronic inflammation develops when the stimulus persists or tissue damage continues. It is characterised by the presence of macrophages and lymphocytes, leading to tissue remodelling and sometimes scarring.
While acute inflammation aids healing, chronic inflammation can cause long-term tissue damage if not resolved.
Blood clots not only prevent blood loss but also act as a temporary barrier to infection by sealing the wound.
They form a physical plug of fibrin and trapped cells that prevents pathogens from entering the bloodstream.
Furthermore, platelets release growth factors that promote angiogenesis (new blood vessel formation) and tissue regeneration, accelerating wound repair once the immediate danger of infection has passed.
Practice Questions
Question 1 (2 marks)
Describe how the skin and mucus act as primary non-specific defences against pathogen entry in humans.
Mark Scheme:
1 mark: The skin forms a physical barrier made of keratinised cells that prevent pathogens entering the body.
1 mark: Mucus traps pathogens and particles in airways, and cilia move the mucus towards the throat to be swallowed and destroyed.
Question 2 (5 marks)
Explain the role of inflammation as a non-specific defence mechanism and describe how this response helps to prevent the spread of infection.
Mark Scheme:
1 mark: Mast cells release histamine when tissue is damaged or infected.
1 mark: Histamine causes vasodilation, increasing blood flow to the affected area.
1 mark: Capillary permeability increases, allowing plasma, white blood cells, and antibodies to enter tissues.
1 mark: This leads to swelling, redness, and heat, isolating the pathogens and facilitating immune cell access.
1 mark: Phagocytes are attracted to the site by chemical signals (cytokines) to destroy pathogens and begin tissue repair.

