OCR Specification focus:
‘B and T lymphocytes coordinate via cell signalling (interleukins), with clonal selection and expansion; include plasma cells, T helper, T killer, and B/T memory cells.’
The specific immune response is a highly specialised defence mechanism that recognises and targets particular pathogens. It involves lymphocytes, chemical signalling, and the development of immunological memory, ensuring faster and stronger protection upon future exposure to the same pathogen.
The Nature of the Specific Immune Response
The specific immune response, also known as the adaptive immune response, is slower than non-specific defences but far more precise. It relies on antigens—unique molecules, often proteins or polysaccharides, on a pathogen’s surface—that the immune system identifies as foreign. Each lymphocyte possesses receptors specific to one antigen, enabling a tailored reaction.
Antigen: A molecule, usually a protein or polysaccharide, on the surface of a pathogen that triggers an immune response.
Once an antigen is detected, lymphocytes undergo a process of recognition, activation, clonal selection, and expansion, forming the basis of immunity.
Lymphocytes and Their Roles
There are two primary types of lymphocytes involved in the specific immune response:
B lymphocytes (B cells): mature in the bone marrow and are responsible for producing antibodies.
T lymphocytes (T cells): mature in the thymus and coordinate or directly destroy infected cells.
Each lymphocyte has antigen receptors specific to one antigen. When an antigen binds to the correct receptor, it triggers a cascade of cellular events leading to the activation of the immune response.
Antigen Presentation and Recognition
The immune response begins when a phagocyte, such as a macrophage or dendritic cell, engulfs a pathogen through phagocytosis and digests it within lysosomes. Fragments of the pathogen’s antigens are then displayed on the cell surface, creating an antigen-presenting cell (APC).
Antigen-presenting cell (APC): A cell that displays foreign antigens on its surface to activate specific lymphocytes.
This presentation is crucial for initiating the specific immune response. APCs travel to the lymph nodes, where they encounter T lymphocytes with complementary receptors.
Activation of T Lymphocytes
T lymphocytes are central to immune coordination. When a T helper (Th) cell receptor binds to an antigen on an APC, the cell becomes activated. This process requires chemical communication through cytokines, particularly interleukins, which stimulate other immune cells.
Interleukins: A group of signalling proteins (cytokines) secreted by T helper cells that coordinate the activity of the immune system.
Activated T helper cells then perform several essential roles:
Release interleukins to stimulate B cells for antibody production.
Activate T killer cells (cytotoxic T cells) to destroy infected host cells.
Promote phagocyte activity to enhance pathogen clearance.
Clonal Selection and Clonal Expansion
The principle of clonal selection ensures that only lymphocytes with receptors complementary to the specific antigen are activated. These selected cells then undergo clonal expansion, multiplying rapidly through mitosis to form a large population of identical cells.
Clonal selection: The activation of a specific lymphocyte whose receptor matches a pathogen’s antigen.
Once selected, lymphocytes proliferate into distinct types with specialised functions.
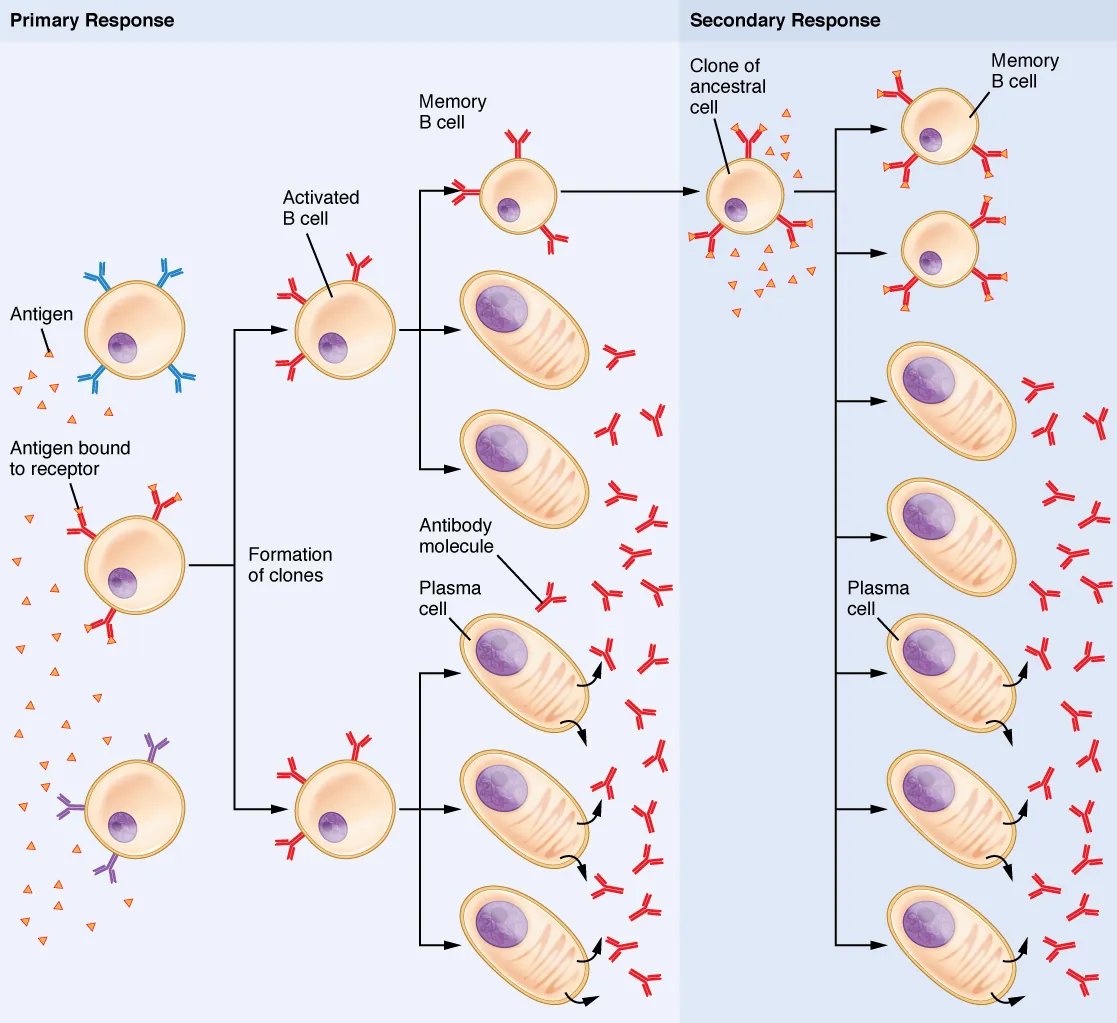
Clonal selection of B lymphocytes during the primary response produces short-lived plasma cells and long-lived B memory cells. Upon re-exposure, memory cells rapidly differentiate, driving a larger secondary response. The diagram emphasises selection of antigen-specific clones and subsequent expansion. Source.
T Lymphocyte Differentiation
Following activation and clonal expansion, T lymphocytes differentiate into specific subtypes:
T helper (Th) cells: release cytokines to activate B cells and other immune components.
T killer (cytotoxic T, Tc) cells: directly destroy infected body cells by releasing perforin, which creates pores in the target cell membrane.
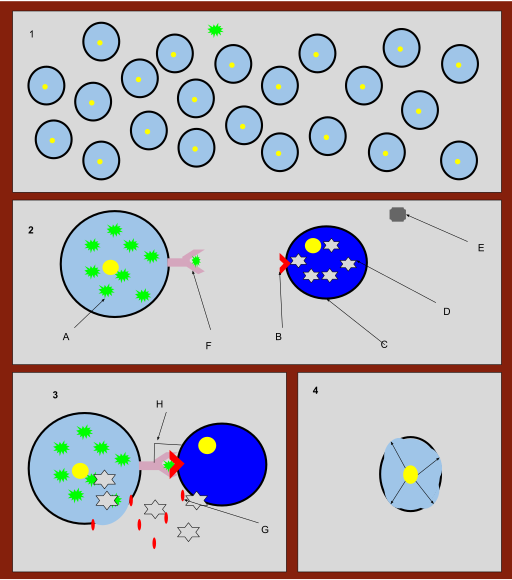
A cytotoxic T cell (CD8⁺) engages an infected cell and releases perforin and associated enzymes to induce apoptosis in the target. The diagram emphasises receptor recognition and perforin-mediated membrane disruption. Extra labels such as lymphotoxin are present but not required for OCR. Source.
T regulator (Tr) cells: suppress the immune response after the pathogen is eliminated to prevent autoimmune reactions.
T memory (Tm) cells: remain in the bloodstream to provide long-term immunity, enabling a rapid secondary response.
The B Lymphocyte Response
When activated by both antigen binding and signals from T helper cells, B cells begin their part of the immune response. The process involves:
Antigen recognition – B cells bind to the specific antigen on a pathogen.
Activation by T helper cells – interleukins from Th cells stimulate the B cell.
Clonal expansion – the activated B cell divides into many identical cells.
Differentiation into:
Plasma cells: short-lived cells that secrete large quantities of antibodies specific to the antigen.
B memory cells: long-lived cells that remain dormant until the same antigen reappears.
Plasma cell: A differentiated B lymphocyte that produces and secretes antibodies specific to a particular antigen.
Antibodies neutralise pathogens, act as opsonins to mark them for destruction, and can cause agglutination of pathogens, aiding phagocytosis.
Immunological Memory and the Secondary Response
One of the defining features of the specific immune response is the formation of immunological memory. Following an infection:
B memory cells and T memory cells persist in the body for years.
Upon reinfection with the same pathogen, these memory cells recognise the antigen immediately.
They rapidly divide and activate plasma cells and cytotoxic T cells, producing antibodies far more quickly than during the first exposure.
This leads to the secondary immune response, which is faster and more intense, often preventing the onset of symptoms.
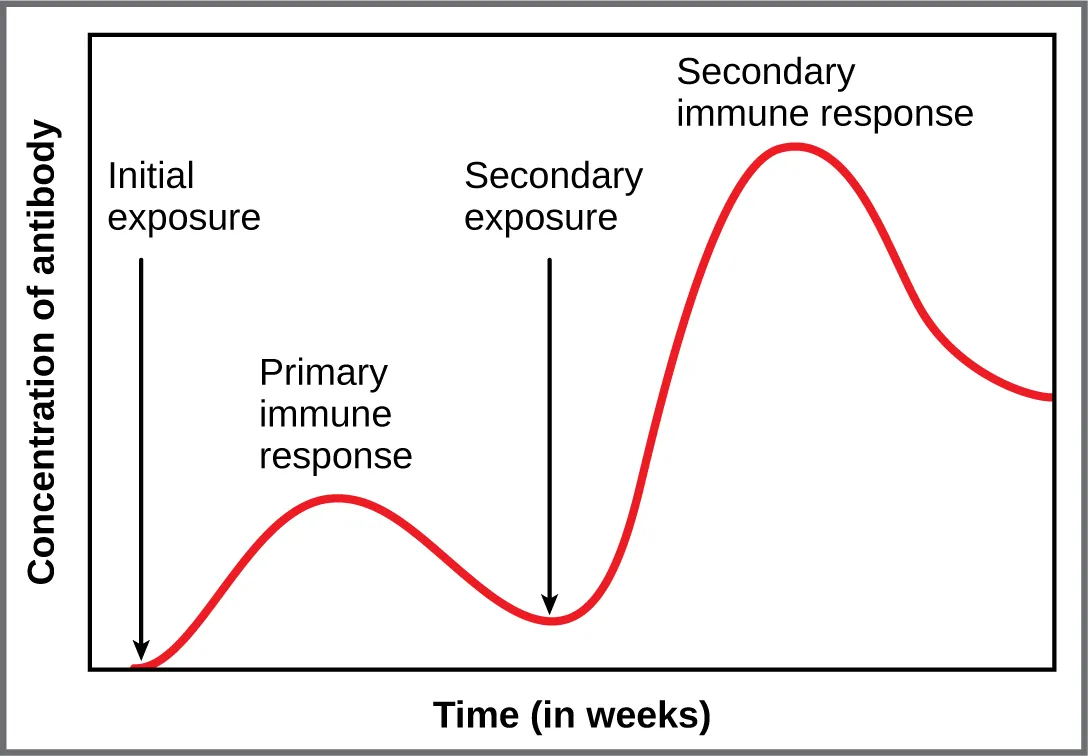
Graph comparing antibody concentration over time after first and second exposure to the same antigen. The secondary response is more rapid and reaches a higher titre due to B and T memory cells. This visual closely aligns with OCR’s requirement to understand immunological memory. Source.
Immunological memory: The capacity of the immune system to respond more rapidly and effectively to pathogens it has encountered before.
Overview of Coordination and Communication
The effectiveness of the specific immune response depends on precise coordination between its cellular components:
T helper cells serve as the central communicators.
Interleukins act as messengers to activate B cells, T killer cells, and phagocytes.
Feedback control by T regulator cells prevents overreaction once the threat is eliminated.
This complex interplay of recognition, selection, and memory ensures that the body can mount targeted and lasting protection against future infections.
FAQ
T helper cells recognise antigens through their T cell receptors (TCRs), which bind specifically to antigens presented on MHC class II molecules of antigen-presenting cells (APCs).
This interaction requires a co-receptor (CD4) on the T helper cell to stabilise the binding. Once bound, the T helper cell is activated and begins secreting interleukins, coordinating the rest of the immune response.
Only antigens processed and displayed by APCs can activate T helper cells—free antigens in body fluids cannot.
Clonal selection ensures that only lymphocytes specific to foreign antigens are activated. During lymphocyte development in the bone marrow and thymus, cells that respond to self-antigens are eliminated through negative selection.
If this process fails, self-reactive lymphocytes could survive and trigger immune responses against the body’s own tissues, leading to autoimmune diseases such as rheumatoid arthritis or type 1 diabetes.
Activated T helper cells release interleukins that bind to receptors on B cells.
The specific signals depend on:
The cytokine type and concentration, which determine the differentiation pathway.
The antigen exposure duration, as prolonged stimulation favours memory cell formation.
The cellular environment in the lymph node, influencing whether the B cell becomes a plasma cell (short-term antibody production) or a B memory cell (long-term immunity).
Cytotoxic T (Tc) cells recognise infected host cells displaying foreign antigens on MHC class I molecules. Once bound, they release perforin, a protein that forms pores in the target cell’s membrane.
Through these pores, granzymes—enzymes that trigger programmed cell death (apoptosis)—enter the cell, ensuring the infection is contained without bursting the cell and spreading pathogens.
During the primary response, naïve B and T cells must first locate their complementary antigens, a process that takes several days. Antibody levels rise slowly and decline after the pathogen is cleared.
In the secondary response, memory cells are already present. They rapidly:
Recognise the antigen.
Undergo clonal expansion without requiring T helper cell activation.
Produce large quantities of high-affinity antibodies quickly.
This molecular efficiency explains why reinfection often produces no symptoms.
Practice Questions
Question 1 (2 marks)
Explain the role of T helper cells in the specific immune response.
Mark Scheme:
1 mark for stating that T helper cells release cytokines/interleukins to activate other immune cells.
1 mark for specifying that they stimulate B cells to produce antibodies and/or activate T killer cells or phagocytes.
(Max 2 marks)
Question 2 (5 marks)
Describe how the specific immune response leads to immunological memory and explain how this provides protection against future infection by the same pathogen.
Mark Scheme:
1 mark: Recognition of specific antigens by lymphocytes with complementary receptors.
1 mark: Explanation of clonal selection and clonal expansion of specific B and T lymphocytes.
1 mark: Reference to formation of plasma cells that produce antibodies during the primary response.
1 mark: Reference to formation of B and T memory cells that remain in the body after infection.
1 mark: Description of faster and stronger secondary response upon reinfection (rapid antibody production preventing symptoms).
(Max 5 marks)

