OCR Specification focus:
‘Explain vaccination principles and programmes, reasons for updates; sources of medicines from microorganisms and plants; widespread antibiotic use and rising resistance with implications for healthcare.’
Vaccinations, medicines and antibiotics are essential components of disease prevention and treatment. Understanding how they work, their origins, and modern challenges such as resistance is vital for biology.
Vaccination Principles
Vaccination is the deliberate introduction of antigenic material to stimulate the immune system and provide protection against a specific pathogen without causing the disease itself.
Vaccination: The administration of an antigenic material to stimulate an immune response and produce immunological memory without causing disease.
How Vaccination Works
When a vaccine is introduced into the body, the specific immune response is activated:
Antigens from the pathogen are recognised by B and T lymphocytes.
Clonal selection and clonal expansion occur, producing plasma cells that secrete antibodies and memory cells.
On subsequent exposure to the real pathogen, memory cells enable a secondary immune response that is faster and stronger, preventing illness.
Types of Vaccines
Different vaccine types stimulate immunity in various ways:
Attenuated (live) vaccines: contain weakened pathogens (e.g. measles, mumps, rubella).
Inactivated vaccines: contain killed pathogens (e.g. influenza).
Toxoid vaccines: use inactivated bacterial toxins (e.g. tetanus).
Subunit or recombinant vaccines: contain only specific antigens (e.g. HPV).
mRNA vaccines: use genetic code for an antigen (e.g. COVID-19 mRNA vaccines).
Each type aims to expose the immune system safely to pathogen-specific antigens to trigger lasting immunity.
Vaccination Programmes
Vaccination programmes are vital for public health and herd immunity — the indirect protection of unvaccinated individuals when a high proportion of the population is immune.
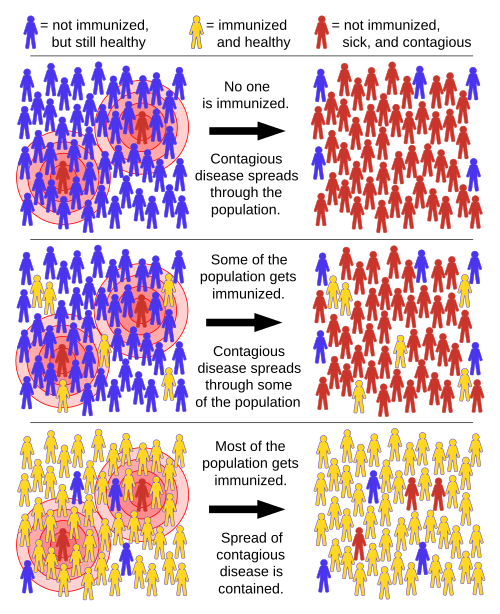
A schematic of herd immunity showing transmission when no one is immunised, when some are immunised (insufficient coverage), and when a critical proportion is immunised. The diagram illustrates how vaccination interrupts chains of transmission, protecting unvaccinated individuals. Labels are concise and appropriate for OCR A-Level coverage. Source.
Key features include:
Mass immunisation: widespread vaccination reduces disease incidence.
Booster doses: maintain immunity over time.
Targeted programmes: specific groups (e.g. infants, elderly) receive vaccines based on vulnerability.
Global initiatives: the World Health Organization (WHO) coordinates efforts such as eradication of smallpox and control of polio.
Reasons for Vaccine Updates
Vaccines must be periodically updated due to pathogen antigenic variation.
Antigenic variation: The process by which pathogens alter their surface antigens, enabling them to evade recognition by the immune system.
This variation is particularly common in viruses such as influenza, where mutations alter antigenic sites, rendering previous vaccines less effective. Annual reviews of influenza strains are therefore necessary to design updated vaccines that match circulating variants.
Medicines from Microorganisms and Plants
Natural Sources of Medicines
Many medicines originate from natural biological sources, particularly microorganisms and plants, which produce bioactive compounds for defence.
Examples include:
Penicillin from the fungus Penicillium chrysogenum, the first true antibiotic discovered by Alexander Fleming.
Aspirin derived from salicylic acid found in willow bark, used as an anti-inflammatory and pain reliever.
Morphine extracted from the opium poppy (Papaver somniferum) and used as a potent analgesic.
Taxol (paclitaxel) from the Pacific yew tree, used in cancer treatment.
Artemisinin from the plant Artemisia annua, effective against malaria.
Scientists continue to explore bioprospecting — the search for new medicinal compounds in natural sources such as rainforests and marine environments.
Synthetic Biology and Drug Development
Modern biotechnology allows the modification of microorganisms to produce medicines more efficiently.
Genes coding for useful compounds are inserted into bacteria, which then synthesise the desired product.
Insulin, for example, is now produced by genetically engineered E. coli, replacing animal-derived sources.
This approach enables sustainable and scalable drug production while reducing environmental impact.
Antibiotics and Their Action
Antibiotics are chemicals that inhibit or kill bacteria without harming host cells.
Antibiotic: A substance produced by microorganisms that kills or inhibits the growth of bacteria.
Modes of Action
Antibiotics target specific bacterial structures or processes:
Cell wall synthesis inhibitors (e.g. penicillin) prevent peptidoglycan cross-linking, causing lysis.
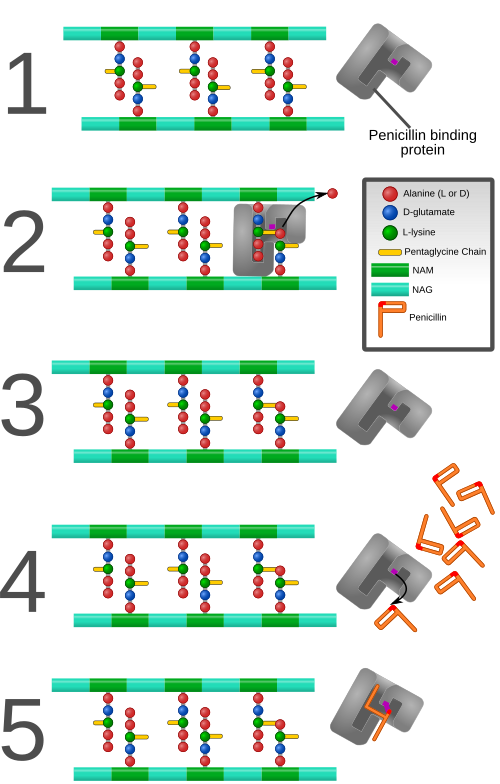
Labeled diagram of PBPs catalysing peptidoglycan cross-links and their suicide inhibition by penicillin’s β-lactam ring. This visual clarifies why actively growing bacteria are susceptible and links structure to function. All labels are clean and syllabus-appropriate. Source.
Protein synthesis inhibitors (e.g. tetracyclines) bind to bacterial ribosomes, blocking translation.
Nucleic acid synthesis inhibitors (e.g. ciprofloxacin) disrupt DNA replication.
Cell membrane disruptors (e.g. polymyxins) alter membrane permeability.
Each antibiotic type has a specific mode of action, making it crucial to match the drug to the infection.
Antibiotic Resistance
Widespread use and misuse of antibiotics have accelerated the evolution of antibiotic-resistant bacteria.
Antibiotic resistance: The ability of bacteria to survive and reproduce in the presence of an antibiotic that would normally kill or inhibit them.
Resistance arises through genetic mutations or acquisition of resistance genes via horizontal gene transfer (plasmids).
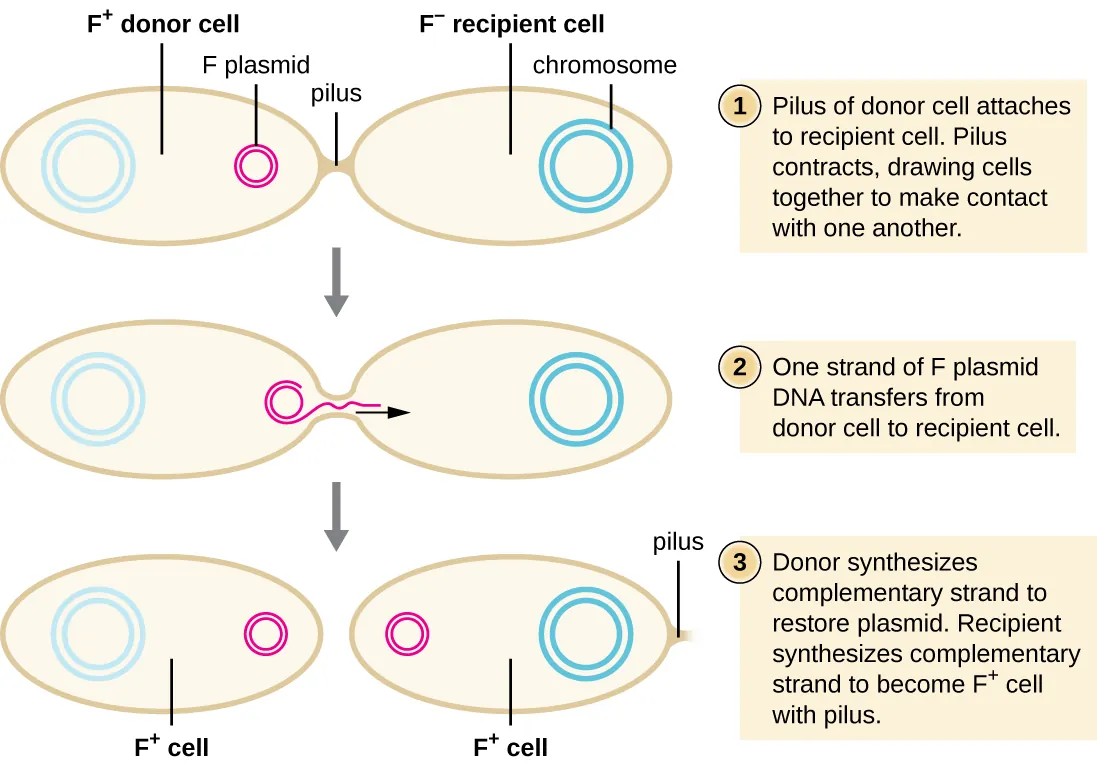
Stepwise, labelled diagram of F-plasmid conjugation: pilus contact, cell pairing, single-strand transfer, and synthesis of complementary strands. This explains how resistance plasmids propagate through bacterial populations. The figure is focused on conjugation only; no unnecessary detail is included. Source.
Over time, selection pressure favours resistant strains, which proliferate.
Examples include:
MRSA (Methicillin-resistant Staphylococcus aureus)
C. difficile (Clostridium difficile)
Multi-drug-resistant tuberculosis (MDR-TB)
These infections are difficult to treat, leading to prolonged illness and higher healthcare costs.
Implications for Healthcare
Antibiotic resistance poses a major global health threat. Hospitals implement infection control measures such as screening, isolation, and strict hygiene.
To combat resistance, strategies include:
Limiting unnecessary antibiotic prescriptions.
Completing prescribed courses to prevent survival of resistant bacteria.
Developing new antibiotics and alternative therapies, including bacteriophages.
Educating the public and healthcare professionals about responsible use.
International collaboration and ongoing research are essential to preserve antibiotic efficacy for future generations.
FAQ
Adjuvants are substances added to vaccines to boost the body’s immune response to the antigen. They do not provide immunity themselves but help by increasing the antigen’s visibility to the immune system.
They can:
Prolong the antigen’s presence at the injection site.
Stimulate local inflammation, attracting antigen-presenting cells.
Enhance activation of T helper cells, leading to stronger B cell and antibody responses.
Common adjuvants include aluminium salts and oil-in-water emulsions used in several modern vaccines.
Antibiotics target structures and processes unique to bacteria, such as cell walls, ribosomes, and metabolic pathways. Viruses lack these features because they rely on a host cell’s machinery to replicate.
Since viruses exist mainly as nucleic acid inside a protein coat, antibiotics have no biochemical targets to disrupt. Treating viral infections therefore requires antiviral drugs that block viral entry, replication, or release rather than bacterial processes.
Bactericidal antibiotics kill bacteria directly, often by disrupting cell wall formation (e.g. penicillin) or damaging membranes.
Bacteriostatic antibiotics inhibit bacterial growth or reproduction, allowing the immune system to clear the infection (e.g. tetracycline).
The choice between them depends on the infection type, the patient’s immune status, and the site of infection. For severe systemic infections, bactericidal antibiotics are often preferred for rapid bacterial clearance.
Researchers isolate microorganisms from diverse environments, such as soil or marine sediments, and culture them under different conditions to encourage production of novel bioactive compounds.
Key steps include:
Screening for antimicrobial activity against known pathogens.
Purifying and characterising the active compounds chemically.
Testing for safety, stability, and spectrum of activity.
Advances in genomic sequencing and synthetic biology now allow identification and modification of gene clusters responsible for antibiotic production, leading to the discovery of new or improved drugs.
Successful programmes rely on a combination of biological, logistical, and social factors:
High vaccine efficacy and appropriate dosing schedules.
Cold chain systems to maintain vaccine stability during transport.
Public trust and education to encourage participation and counter misinformation.
International coordination through organisations such as the World Health Organization (WHO) and UNICEF.
These factors together ensure high coverage rates, which are essential for achieving herd immunity and preventing disease outbreaks.
Practice Questions
Question 1 (2 marks)
Explain how vaccination leads to the development of immunity in an individual.
Mark scheme:
(1 mark) The vaccine introduces antigens from a pathogen into the body.
(1 mark) This stimulates the specific immune response, producing memory cells that enable a faster and stronger response upon reinfection.
Question 2 (5 marks)
Antibiotic resistance is a growing problem in healthcare. Describe how antibiotic resistance arises in bacterial populations and outline two strategies that can be used to reduce its spread.
Mark scheme:
(1 mark) Resistance arises due to random mutations in bacterial DNA or by acquiring resistance genes via horizontal gene transfer (e.g. conjugation).
(1 mark) Antibiotics act as a selection pressure, killing susceptible bacteria and allowing resistant ones to survive and reproduce.
(1 mark) Resistant alleles are passed on to offspring, increasing the proportion of resistant bacteria in the population.
(1 mark) One strategy: limit unnecessary antibiotic prescriptions or ensure full completion of antibiotic courses to prevent survival of resistant bacteria.
(1 mark) Second strategy: develop new antibiotics or use infection control measures (e.g. hygiene, isolation) to prevent spread of resistant strains.

