OCR Specification focus:
‘Relate the distribution of tissues in arteries, arterioles, capillaries, venules and veins to their functions in pressure control, exchange and return of blood.’
Blood vessels form the essential transport network of the circulatory system, ensuring efficient delivery of oxygen, nutrients and hormones, while removing carbon dioxide and waste from tissues and organs.
Structure and Function of Blood Vessels
Blood vessels vary structurally to meet their specific functional demands, from maintaining high pressure in arteries to facilitating diffusion in capillaries and ensuring return flow in veins.
1. The General Vessel Wall Structure
All blood vessels (except capillaries) share a similar basic structure composed of three layers:
Tunica intima – the innermost lining made of endothelium, a single layer of smooth, flattened endothelial cells that reduces friction and provides a smooth surface for blood flow.
Tunica media – a middle layer of smooth muscle and elastic fibres responsible for controlling vessel diameter and withstanding pressure changes.
Tunica externa (adventitia) – an outer coat of collagen fibres providing strength and structural support, preventing over-expansion of the vessel.
Endothelium: A thin layer of specialised squamous epithelial cells lining the interior of blood vessels, forming a smooth surface to minimise resistance to blood flow.
Each vessel type varies the thickness and composition of these layers to fulfil its role in the circulatory pathway.
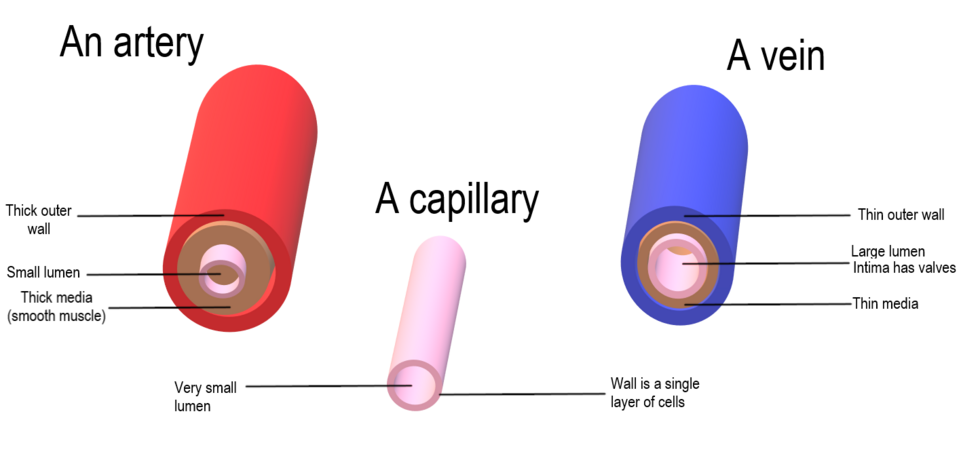
Labeled cross-sections compare an artery, capillary, and vein, highlighting tunica intima, tunica media, tunica externa and lumen size. The thicker muscular and elastic media in arteries supports high pressure, the single-cell wall of capillaries minimises diffusion distance, and the thin-walled, large-lumen vein facilitates low-pressure return. The diagram stays within syllabus scope without unnecessary extra anatomy. Source.
2. Arteries: Structure for High Pressure Transport
Arteries carry blood away from the heart at high pressure and therefore require strong, elastic walls.
Key structural adaptations:
Thick tunica media with abundant elastic fibres to withstand and smooth out pressure surges from ventricular systole.
Smooth muscle allows for vasoconstriction (narrowing) and vasodilation (widening), regulating blood flow and pressure.
Small lumen relative to wall thickness maintains high blood pressure.
Collagen fibres in the outer layer prevent rupture during pressure peaks.
During each heartbeat, the elastic recoil of arteries helps maintain continuous blood flow even when the heart relaxes.
Vasoconstriction: The contraction of smooth muscle in the arterial wall, narrowing the vessel lumen to increase blood pressure and reduce blood flow.
Between contractions, arteries return to their original diameter, a property called elastic recoil, maintaining pressure throughout the circulation.
3. Arterioles: Control Points for Blood Distribution
Arterioles are smaller branches of arteries that regulate blood flow into capillary beds.
Features and functions:
Possess a relatively thicker layer of smooth muscle compared with their size, enabling fine control of blood flow to tissues.
Less elastic tissue than arteries as blood pressure has already decreased.
Can divert blood to specific organs through constriction or dilation in response to local oxygen demand, temperature or sympathetic nervous input.
Precapillary sphincter: A ring of smooth muscle at the entrance to a capillary bed that contracts or relaxes to control blood flow into the capillaries.
Arterioles therefore play a crucial role in thermoregulation and the distribution of oxygenated blood during varying physiological states.
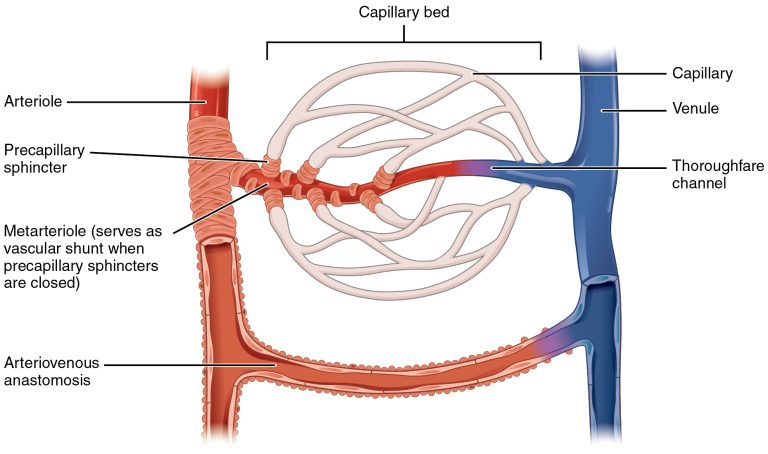
A capillary bed fed by a metarteriole demonstrates how precapillary sphincters regulate entry into true capillaries. When sphincters close, blood is shunted via the thoroughfare channel/arteriovenous anastomosis, illustrating control of tissue perfusion. This figure contains only syllabus-appropriate features for OCR. Source.
4. Capillaries: Sites of Exchange
Capillaries are the exchange vessels where diffusion of gases, nutrients and wastes occurs between blood and tissues.
Structural characteristics enabling efficient exchange:
Very thin walls – composed of a single layer of endothelial cells (one cell thick) to minimise diffusion distance.
Extensive networks (capillary beds) create a large surface area for exchange.
Narrow lumen (about 7 μm) ensures close contact between red blood cells and capillary walls for efficient oxygen transfer.
Slow blood flow due to high total cross-sectional area, providing sufficient time for diffusion.
Diffusion gradient: The difference in concentration across a membrane that drives the passive movement of molecules such as oxygen or carbon dioxide.
Some capillaries are fenestrated, having small pores that allow faster transfer of larger molecules such as hormones or plasma proteins, particularly in organs like the kidneys.
5. Venules: Collecting Blood from Capillaries
Venules are small vessels that collect blood from capillary beds and transport it to larger veins.
Key features:
Thin walls with little smooth muscle and few elastic fibres since pressure is much lower than in arterioles.
Permeable endothelium allows white blood cells to exit into tissues during immune responses.
Gradually merge to form veins as they carry blood back toward the heart.
Venules act as the transition point between the exchange system of capillaries and the return system of veins.
6. Veins: Return Vessels at Low Pressure
Veins carry blood back to the heart under low pressure, often against gravity, particularly from the lower body.
Structural adaptations:
Thin tunica media with fewer smooth muscle and elastic fibres, as pressure fluctuations are minimal.
Large lumen reduces resistance to flow.
Valves prevent backflow of blood, especially in limbs.
Skeletal muscle contractions and respiratory movements aid venous return by squeezing veins and increasing pressure differentials.
Venous return: The flow of blood back to the heart via the veins, assisted by skeletal muscle contraction, breathing movements, and one-way valves.
Superficial veins in the limbs and deep veins within muscles rely heavily on this muscular and valve mechanism to maintain continuous circulation.
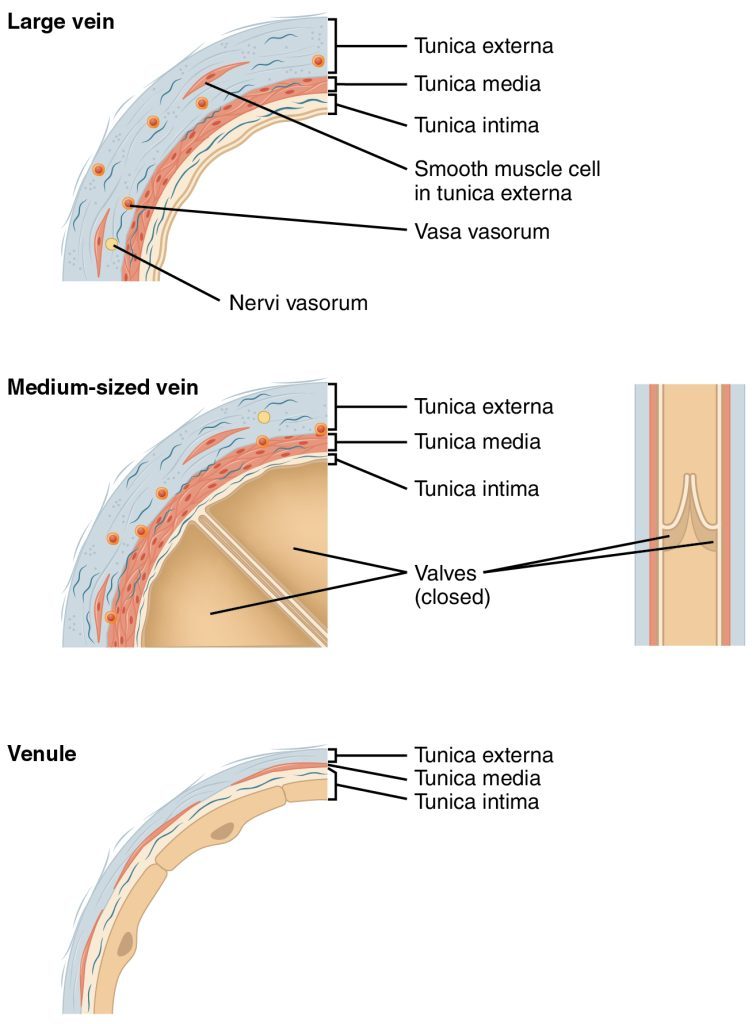
Comparative sections of a large vein, medium-sized vein, and venule show thin media, thick externa, and the presence of venous valves that enforce unidirectional flow. It visually supports the structure–function link for low-pressure venous return described in the notes. The panel includes nervi vasorum/vasa vasorum labels—useful context but slightly beyond the strict syllabus emphasis. Source.
7. Relationships Between Vessel Structure and Function
Arteries: Thick, elastic and muscular walls maintain high pressure to deliver blood rapidly from the heart.
Arterioles: Adjust resistance and flow distribution through contraction or relaxation of smooth muscle.
Capillaries: Thin walls and slow flow maximise exchange efficiency between blood and tissues.
Venules and Veins: Thin, distensible walls with valves allow low-pressure return of blood to the heart without backflow.
Each vessel’s structure reflects its role in maintaining pressure control, enabling efficient exchange, and ensuring continuous circulation throughout the body.
FAQ
Elastic arteries, such as the aorta, contain a high proportion of elastic fibres in their tunica media. These fibres allow the vessel to stretch during systole and recoil during diastole, maintaining continuous blood flow despite pulsatile pressure.
Muscular arteries, found further from the heart, have more smooth muscle and fewer elastic fibres. This structure enables precise regulation of blood flow to specific organs by vasoconstriction and vasodilation rather than energy storage and release.
Veins experience much lower blood pressure than arteries. A larger lumen reduces resistance to flow and allows greater blood volume to return to the heart without requiring high pressure.
Additionally, the wider lumen accommodates the slow-moving, low-pressure blood returning from tissues, while valves prevent backflow. This structure helps veins act as a blood reservoir, holding around 60–70% of total blood volume at rest.
The vasa vasorum are small blood vessels that supply oxygen and nutrients to the outer layers of large arteries and veins.
In large vessels, the wall is too thick for diffusion from the lumen to meet metabolic needs in the outer tunics.
They supply the tunica media and externa with oxygen and nutrients.
They are especially important in elastic arteries (like the aorta) and large veins, which have thick walls.
Smaller vessels lack vasa vasorum because diffusion from the lumen is sufficient for their metabolic requirements.
Arterioles, sometimes called resistance vessels, play a crucial role in controlling systemic blood pressure by adjusting their diameter.
Vasoconstriction increases resistance, reducing blood flow to certain areas and raising overall blood pressure.
Vasodilation decreases resistance, increasing blood flow and lowering blood pressure.
This regulation is influenced by the autonomic nervous system and local chemical signals (e.g. CO₂, O₂ levels). The arterioles therefore maintain homeostasis by balancing tissue demand and systemic pressure.
Besides valves, several mechanisms support blood flow back to the heart under low pressure:
Skeletal muscle pump: Contraction of surrounding muscles compresses veins, pushing blood toward the heart.
Respiratory pump: During inspiration, thoracic pressure drops while abdominal pressure rises, drawing blood upward.
Smooth muscle tone: Contraction in vein walls provides a small but steady propulsion.
Gravity: Assists venous return from areas above the heart, such as the head and neck.
Together, these mechanisms ensure efficient venous return, even from lower parts of the body.
Practice Questions
Question 1 (2 marks)
Explain how the structure of a capillary is adapted for its function as an exchange surface.
Mark Scheme:
1 mark for stating that the capillary wall is one cell thick (single layer of endothelial cells), providing a short diffusion distance.
1 mark for stating that capillaries have a narrow lumen or large total surface area, ensuring close contact with tissues and slow blood flow for efficient exchange.
Question 2 (5 marks)
Describe and explain how the structures of arteries and veins are related to their functions in the circulatory system.
Mark Scheme:
1 mark for stating that arteries have thick, muscular and elastic walls to withstand and maintain high blood pressure.
1 mark for describing elastic recoil in arteries that helps to smooth pressure fluctuations and maintain continuous flow.
1 mark for stating that veins have thinner walls with less smooth muscle and elastic tissue, as blood pressure is lower.
1 mark for stating that veins contain valves to prevent backflow of blood.
1 mark for explaining that skeletal muscle contractions or respiratory movements aid venous return, helping blood flow back to the heart under low pressure.

