OCR Specification focus:
‘Describe pressure changes and valve roles during atrial and ventricular events; use heart rate and stroke volume to calculate cardiac output.’
The Cardiac Cycle and Cardiac Output
The cardiac cycle is the sequence of events that occur during one heartbeat, involving the rhythmic contraction and relaxation of the atria and ventricles to pump blood effectively. This process ensures continuous circulation throughout the body.
Overview of the Cardiac Cycle
The cardiac cycle lasts approximately 0.8 seconds in a healthy adult at rest and is divided into three main phases: atrial systole, ventricular systole, and diastole. These phases ensure the unidirectional flow of blood through the heart, controlled by pressure changes and the action of heart valves.
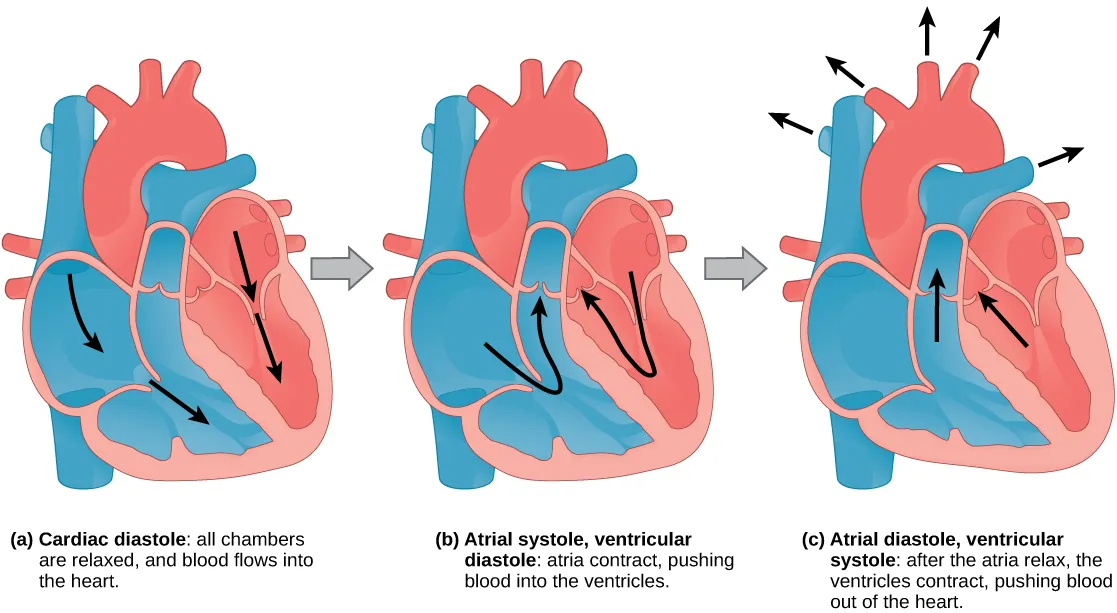
Three-panel diagram of the cardiac cycle: (a) cardiac diastole with AV valves open and semilunar valves closed; (b) atrial systole topping up ventricular filling; (c) ventricular systole ejecting blood as semilunar valves open. The layout mirrors the three-phase description used in your notes. Source.
Atrial Systole
Atrial systole occurs when the atria contract, forcing blood into the ventricles through the atrioventricular (AV) valves (tricuspid and bicuspid/mitral).
The ventricles are already about 70% full due to passive filling; atrial contraction adds the remaining 30%.
The AV valves are open because atrial pressure exceeds ventricular pressure, ensuring efficient blood transfer.
Ventricular Systole
After a short delay, the ventricles contract, beginning ventricular systole.
This contraction causes a sharp rise in ventricular pressure, which forces the AV valves to close — preventing backflow into the atria.
When ventricular pressure exceeds arterial pressure in the aorta and pulmonary artery, the semilunar valves open, allowing blood to be ejected.
The right ventricle pumps blood to the lungs, and the left ventricle pumps blood into the aorta for systemic circulation.
Diastole
During diastole, both atria and ventricles relax.
Ventricular pressure drops below arterial pressure, causing the semilunar valves to close, preventing backflow from the arteries.
As atrial pressure rises due to blood returning to the heart, the AV valves reopen, and passive ventricular filling begins once more.
This phase ensures the heart chambers refill and prepares the heart for the next beat.
Valve Function and Pressure Relationships
Valves play a critical role in maintaining one-way flow within the heart by responding to pressure differences between chambers and vessels.
Atrioventricular (AV) Valves
Located between atria and ventricles.
Tricuspid valve (right side) and bicuspid/mitral valve (left side).
Close when ventricular pressure exceeds atrial pressure, producing the first heart sound (“lub”).
Semilunar Valves
Found at the exits of the aorta and pulmonary artery.
Open when ventricular pressure rises above arterial pressure and close when it falls below it.
Closure produces the second heart sound (“dub”).
These coordinated valve actions prevent regurgitation and maintain efficient flow through the pulmonary and systemic circuits.
Pressure Changes During the Cardiac Cycle
The cardiac cycle involves continuous changes in pressure within the atria, ventricles, and major arteries.
During atrial systole, atrial pressure briefly increases as the atria contract.
During ventricular systole, ventricular pressure rises steeply, peaking during blood ejection.
Aortic pressure rises as blood enters from the left ventricle, then gradually declines during diastole as elastic recoil maintains arterial flow.
Pressure variations ensure that blood always flows from regions of higher pressure to lower pressure, driving circulation through the heart.
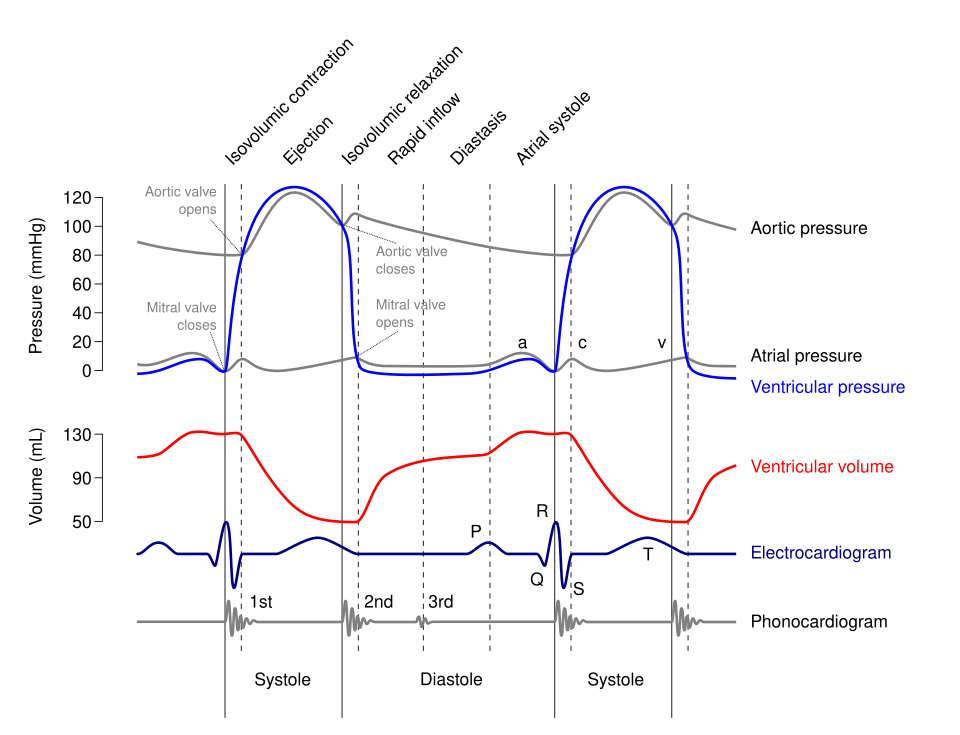
Wiggers diagram displaying atrial, ventricular, and aortic pressure curves through atrial systole, ventricular systole, and diastole, with AV and semilunar valve status and S1/S2 timing. This visual directly links pressure changes to valve actions. The ECG and phonocardiogram traces are included for context but extend beyond the OCR requirement. Source.
Electrical Coordination and Timing
Although this subtopic focuses on mechanical events, it’s important to note that the cardiac cycle is initiated by electrical impulses from the sinoatrial node (SAN).
This electrical control ensures that atrial contraction precedes ventricular contraction, allowing optimal ventricular filling before ejection.
Cardiac Output
Cardiac output (CO) is the total volume of blood pumped by one ventricle per minute. It is a key indicator of cardiac performance and circulatory efficiency.
EQUATION
—-----------------------------------------------------------------
Cardiac Output (CO) = Stroke Volume (SV) × Heart Rate (HR)
CO = volume of blood pumped per minute (cm³ min⁻¹ or dm³ min⁻¹)
SV = volume of blood pumped per beat (cm³ or mL)
HR = number of beats per minute (bpm)
—-----------------------------------------------------------------
Typical values:
Resting stroke volume ≈ 70 mL per beat.
Heart rate ≈ 70 bpm.
Therefore, cardiac output ≈ 4.9 L per minute in a healthy adult.
Stroke Volume
Stroke volume is determined by:
Venous return — greater blood return stretches the ventricular walls (Starling’s law of the heart), leading to stronger contraction.
Contractility — influenced by sympathetic stimulation and circulating hormones such as adrenaline.
Afterload — the resistance the ventricles must overcome to eject blood; higher arterial pressure can reduce stroke volume.
Heart Rate
Heart rate is controlled by the autonomic nervous system:
Sympathetic stimulation increases heart rate (via noradrenaline release).
Parasympathetic stimulation (via the vagus nerve) decreases heart rate.
Factors such as exercise, emotion, temperature, and hormones can modify heart rate to meet metabolic demands.
Regulation of Cardiac Output
Maintaining adequate cardiac output is crucial for supplying tissues with oxygen and nutrients. The body dynamically adjusts CO through several mechanisms:
Neural Control
Baroreceptors in the aorta and carotid arteries detect changes in blood pressure.
Chemoreceptors respond to pH and CO₂ levels in the blood.
These receptors send signals to the cardiovascular control centre in the medulla oblongata, which adjusts autonomic output to the heart.
Hormonal and Intrinsic Control
Adrenaline and noradrenaline increase both heart rate and stroke volume during stress or exercise.
The Frank–Starling mechanism ensures that increased venous return results in a stronger contraction, keeping cardiac output proportional to venous inflow.
Significance of Pressure and Volume Relationships
Understanding the interplay between pressure, volume, and valve action is essential to interpreting cardiac function.
A pressure–volume loop can illustrate how ventricular pressure rises during systole, peaks during ejection, and falls during relaxation, with the area enclosed by the loop representing stroke work — the mechanical energy of each heartbeat.
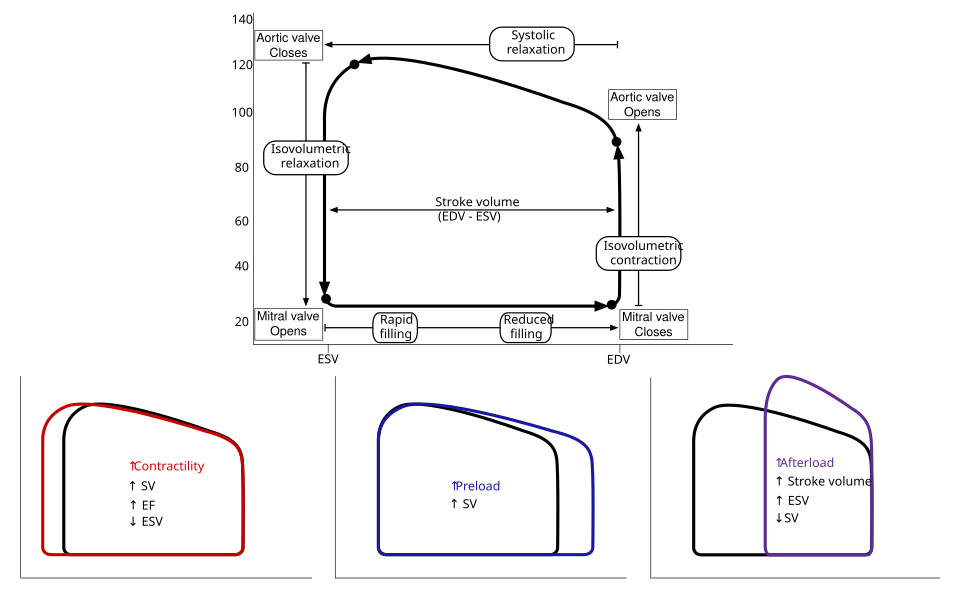
Left-ventricular pressure–volume loop showing isovolumetric contraction, ejection, isovolumetric relaxation, and filling. The width of the loop equals stroke volume, and its position/shape shifts with changes in preload, afterload, and contractility. This figure includes preload/afterload/contractility variants; these are useful extensions but not explicitly required by the OCR syllabus. Source.
Key Points of the Cardiac Cycle
The cardiac cycle ensures coordinated contraction and relaxation of heart chambers for efficient circulation.
Valves maintain unidirectional flow by opening and closing in response to pressure gradients.
Pressure changes within the heart drive blood flow through different chambers and into arteries.
Cardiac output reflects the combined effect of heart rate and stroke volume, adapting to the body’s metabolic demands.
FAQ
The heart sounds are produced by the closure of valves.
The “lub” (S1) is created when the atrioventricular (AV) valves close at the start of ventricular systole.
The “dub” (S2) results from the semilunar valves closing at the start of ventricular diastole.
These sounds are not caused by the valves themselves, but by the vibrations of surrounding tissues and blood as the valves snap shut under pressure differences.
The sequence of events is identical on both sides, but pressures differ due to different circulatory demands.
The left ventricle generates higher pressure to pump blood into the systemic circulation.
The right ventricle operates at lower pressure to supply the pulmonary circuit, preventing lung damage.
Despite these pressure differences, valve timing and cycle duration remain synchronised to maintain efficient blood flow.
Valve faults can lead to stenosis (narrowing) or incompetence (failure to close properly).
Stenosis restricts blood flow, increasing pressure upstream.
Incompetence causes regurgitation, where blood leaks backward.
These conditions alter pressure gradients and can reduce cardiac output, forcing the heart to work harder, often leading to hypertrophy of affected chambers.
As heart rate increases, the duration of diastole shortens more than systole.
This ensures that blood can still be ejected effectively, but ventricular filling time decreases.
To compensate:
Venous return increases due to muscle and respiratory pump effects.
Stronger atrial contractions and enhanced ventricular elasticity help maintain stroke volume.
At extremely high heart rates, filling may become insufficient, reducing cardiac efficiency.
The left ventricle must overcome the systemic arterial pressure, which is far higher than pulmonary pressure.
It has a thicker muscular wall, producing greater contractile force.
The right ventricle pumps blood to the lungs, where resistance is low, so it develops less pressure.
This structural and pressure difference ensures that both sides pump equal volumes of blood per cycle but at different pressures suited to their circulatory roles.
Practice Questions
Question 1 (2 marks)
During the cardiac cycle, explain why the atrioventricular (AV) valves close and describe the effect this has on blood flow.
Mark Scheme:
1 mark: AV valves close when ventricular pressure exceeds atrial pressure.
1 mark: This prevents backflow of blood into the atria during ventricular contraction (systole).
Question 2 (5 marks)
Describe and explain how pressure changes within the heart chambers and major blood vessels control the opening and closing of valves during one complete cardiac cycle.
Mark Scheme:
1 mark: Reference to low pressure in atria at the start of diastole, allowing blood to flow in from the veins.
1 mark: AV valves open when atrial pressure exceeds ventricular pressure, enabling ventricular filling.
1 mark: Ventricular systole increases ventricular pressure, causing AV valves to close (preventing backflow) and semilunar valves to open once ventricular pressure exceeds arterial pressure.
1 mark: As the ventricles relax (diastole), ventricular pressure drops below arterial pressure, so semilunar valves close to prevent backflow from the arteries.
1 mark: Correct sequence and clear explanation that valve operation is entirely pressure-driven, maintaining unidirectional blood flow through the heart.

