OCR Specification focus:
‘Explain hydrostatic and oncotic pressures driving fluid movement, and compare the differing compositions of blood plasma, tissue fluid and lymph.’
The formation of tissue fluid and lymph enables efficient exchange between blood and cells, maintaining homeostasis by balancing fluid distribution and nutrient-waste transport through pressure-driven mechanisms.
Structure and Function of the Capillary Network
The capillary network is the site where blood plasma interacts with body tissues. Capillaries are microscopic vessels with thin, permeable walls composed of a single layer of endothelial cells, allowing substances to move between the blood and surrounding cells.
Arterioles deliver blood to capillaries under relatively high hydrostatic pressure.
Venules collect blood from capillaries, returning it to the venous system.
Capillary beds are closely associated with body cells, ensuring efficient diffusion of gases, nutrients, and metabolic wastes.
The movement of fluid in and out of capillaries is governed by a balance between hydrostatic pressure and oncotic pressure.
Forces Driving Tissue Fluid Formation
Hydrostatic Pressure
At the arterial end of the capillary, the blood hydrostatic pressure is high (around 4.3 kPa). This pressure forces plasma—minus large plasma proteins and blood cells—out through the capillary walls into the surrounding interstitial spaces. The resulting fluid is known as tissue fluid.
Hydrostatic Pressure: The pressure exerted by a fluid against the walls of its container or vessel, promoting fluid movement outwards from the blood capillaries into the tissues.
As the blood flows towards the venous end of the capillary, the hydrostatic pressure decreases (to approximately 1.7 kPa) due to friction and fluid loss.
Oncotic Pressure
The oncotic pressure (also known as colloid osmotic pressure) is created by plasma proteins, especially albumin, which remain in the capillary because they are too large to pass through the endothelial membrane.
Oncotic Pressure: The osmotic pressure generated by plasma proteins that draw water into the capillaries from the surrounding tissue fluid by osmosis.
The oncotic pressure is about 3.3 kPa, relatively constant along the capillary. It opposes the hydrostatic pressure, tending to pull water back into the blood.
Balance of Pressures
At the arterial end, the outward hydrostatic pressure (≈4.3 kPa) exceeds the inward oncotic pressure (≈3.3 kPa), resulting in net filtration out of the capillary.
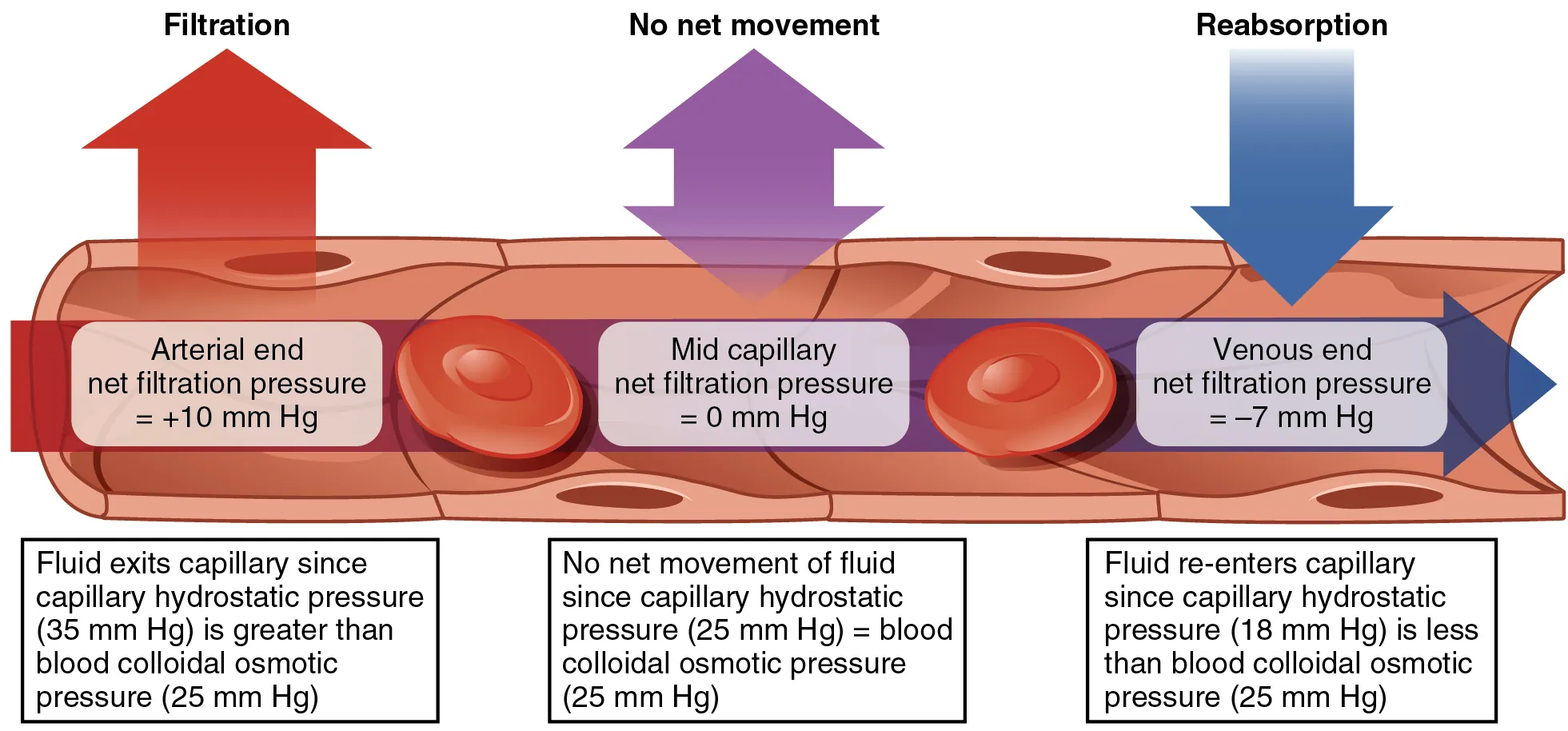
Capillary Exchange — A labelled diagram contrasting CHP and BCOP across a capillary bed. Filtration predominates near the arterial end; reabsorption dominates near the venous end. This directly visualises the balance of forces that generates tissue fluid. Source.
At the venous end, the hydrostatic pressure has fallen (≈1.7 kPa), so oncotic pressure now exceeds hydrostatic pressure, causing net reabsorption of fluid into the capillary.
This dynamic equilibrium maintains effective exchange without excessive fluid loss.
EQUATION
—-----------------------------------------------------------------
Net Filtration Pressure (NFP) = Hydrostatic Pressure (HP) – Oncotic Pressure (OP)
HP = Force driving fluid out of the capillary (kPa)
OP = Force drawing fluid back into the capillary (kPa)
Positive NFP → Filtration (fluid moves out)
Negative NFP → Reabsorption (fluid moves in)
—-----------------------------------------------------------------
Composition and Role of Tissue Fluid
Tissue fluid is essentially blood plasma without plasma proteins or blood cells. It bathes the cells, providing oxygen, glucose, amino acids, and ions, while collecting carbon dioxide and metabolic wastes for removal.
Formed by ultrafiltration from the capillaries at the arterial end.
Acts as an intermediary between the blood and cells, facilitating diffusion of materials.
Returns most of its volume to the capillaries at the venous end due to the osmotic effect of plasma proteins.
Some fluid, however, does not re-enter the blood capillaries and instead enters the lymphatic system.
Formation and Transport of Lymph
Lymph originates as excess tissue fluid that drains into lymphatic capillaries, forming part of the lymphatic system, which ultimately returns fluid to the bloodstream via the thoracic duct and right lymphatic duct.
Lymphatic capillaries have valves preventing backflow and thin, permeable walls to allow fluid entry.
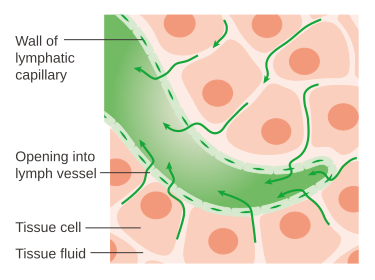
Lymphatic Capillary Mini-valves — Overlapping endothelial cells form one-way flaps that admit tissue fluid when interstitial pressure rises. Anchoring filaments tether the capillary so the lumen opens during tissue expansion. This is the structural basis of lymph formation. Source.
The fluid moves due to skeletal muscle contractions and body movements, since lymph flow is not driven by a pump.
Lymph passes through lymph nodes, where lymphocytes and macrophages remove pathogens, debris, and foreign particles.
Lymph: A clear fluid derived from tissue fluid that circulates through the lymphatic system, transporting immune cells and returning excess interstitial fluid to the bloodstream.
Comparison of Blood Plasma, Tissue Fluid, and Lymph
Each of these fluids represents a stage in the circulation and exchange of materials between the blood and body tissues.
Blood Plasma
Found within blood vessels.
Contains plasma proteins, glucose, amino acids, ions, hormones, and blood cells.
Exerts oncotic pressure due to protein content, particularly albumin.
Tissue Fluid
Located in the interstitial spaces surrounding cells.
Similar composition to plasma but lacks plasma proteins and blood cells.
Provides a medium for exchange of materials between blood and cells.
Lymph
Derived from tissue fluid that enters lymphatic capillaries.
Contains fewer nutrients but higher waste concentration than tissue fluid.
Contains lymphocytes and sometimes fats absorbed from the intestine (forming chyle).
The Role of Pressure Imbalance and Pathology
If the delicate balance between hydrostatic and oncotic pressures is disrupted, fluid accumulation can occur.
Increased capillary hydrostatic pressure, as in high blood pressure, may force more fluid into the tissues, leading to oedema.
Reduced plasma protein levels, such as in liver disease or malnutrition, lower oncotic pressure, impairing reabsorption and also causing oedema.
Lymphatic obstruction, due to infection or surgery, prevents fluid return, resulting in localised swelling.
Such imbalances highlight the importance of homeostatic regulation in maintaining effective tissue perfusion and preventing fluid overload.
Integration with Circulatory Function
The formation of tissue fluid and lymph complements the circulatory system by ensuring that:
Nutrients and gases reach cells efficiently.
Wastes and carbon dioxide are removed effectively.
Immune surveillance is maintained via lymph transport and filtration.
Together, these systems exemplify how hydrostatic and oncotic pressures regulate the continual exchange and recycling of fluids, vital to sustaining multicellular life.
FAQ
Plasma proteins such as albumin and fibrinogen are too large and often carry electrical charges that prevent them from passing through the fenestrations in the capillary endothelium.
Their retention inside the capillaries maintains a high oncotic pressure, ensuring that water is drawn back into the bloodstream at the venous end.
This selective permeability of the capillary wall is essential to prevent excessive loss of solutes and to maintain normal blood osmolarity.
During exercise, arteriolar dilation increases capillary hydrostatic pressure, promoting greater filtration and temporary accumulation of tissue fluid.
However, the rhythmic contractions of skeletal muscles compress lymphatic vessels, propelling lymph towards the thoracic duct and preventing fluid build-up.
As a result, exercise enhances lymphatic return and helps maintain tissue fluid balance despite increased capillary pressure.
Lymphatic vessels contain one-way valves formed by overlapping endothelial flaps.
When interstitial pressure rises, these flaps open to admit fluid; when lymphatic pressure increases internally, the flaps close to prevent backflow.
Additionally, skeletal muscle contractions, respiratory movements, and the pulsation of nearby arteries assist forward lymph movement, ensuring unidirectional flow towards the venous system.
Low plasma protein levels—due to liver disease, protein malnutrition, or kidney damage—reduce oncotic pressure in the blood.
With less osmotic pull to draw water back into capillaries, more fluid remains in the interstitial spaces.
This imbalance between hydrostatic and oncotic forces leads to tissue swelling, known as oedema.
As lymph passes through lymph nodes, it is filtered to remove pathogens, debris, and abnormal cells.
Within these nodes, lymphocytes (especially B and T cells) and macrophages monitor and respond to foreign antigens.
Thus, the lymphatic system not only returns fluid to the bloodstream but also serves as a crucial surveillance network, integrating fluid balance with immune protection.
Practice Questions
Question 1 (2 marks)
Explain how oncotic pressure is generated within the capillaries and describe its role in the formation of tissue fluid.
Mark Scheme:
1 mark for stating that oncotic pressure is generated by plasma proteins (such as albumin) remaining in the blood and not passing through capillary walls.
1 mark for describing that oncotic pressure draws water back into the capillaries from the tissue fluid by osmosis, opposing hydrostatic pressure.
Question 2 (5 marks)
Describe and explain how the balance between hydrostatic pressure and oncotic pressure results in the formation and return of tissue fluid, and outline how the lymphatic system maintains fluid balance in the body.
Mark Scheme:
1 mark for stating that at the arterial end of the capillary, hydrostatic pressure is higher than oncotic pressure, causing fluid to move out of the capillary (filtration).
1 mark for noting that large plasma proteins remain in the blood, maintaining oncotic pressure.
1 mark for explaining that at the venous end, hydrostatic pressure falls below oncotic pressure, so water moves back into the capillary (reabsorption).
1 mark for describing that not all fluid re-enters the capillaries and that excess tissue fluid drains into the lymphatic capillaries.
1 mark for explaining that lymph is returned to the bloodstream via the thoracic duct and right lymphatic duct, maintaining overall fluid balance.

