OCR Specification focus:
‘Endocrine glands secrete hormones into blood; hormones are transported in blood and detected by specific target cells or tissues.’
Endocrine communication is a vital mechanism for coordinating long-term physiological processes. It involves hormones released by endocrine glands that regulate growth, metabolism, and homeostasis through blood transport to target cells.
The Endocrine System
The endocrine system comprises a network of glands that secrete chemical messengers known as hormones directly into the bloodstream. Unlike the nervous system, which transmits signals rapidly via neurones, endocrine communication acts more slowly but exerts prolonged and widespread effects throughout the body.
Endocrine vs. Exocrine Glands
Endocrine glands are specialised structures that release hormones directly into the blood plasma rather than through ducts. Examples include the pituitary gland, thyroid gland, adrenal glands, pancreas (islets of Langerhans), and ovaries or testes.
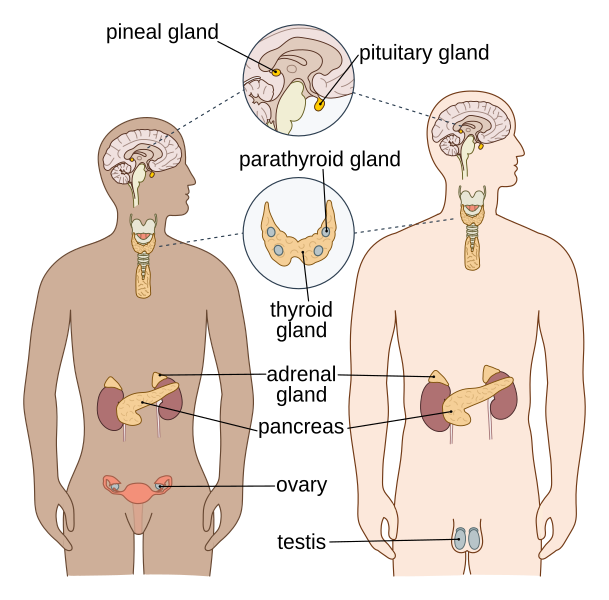
Labelled diagram of the human endocrine system, highlighting major hormone-secreting glands that release chemical messengers into the bloodstream. This visual supports the idea of ductless endocrine organs coordinating body-wide responses. Extra labels (e.g. pineal, parathyroid) are included for anatomical completeness but are not essential to this subsubtopic. Source.
In contrast, exocrine glands release secretions such as enzymes or mucus through ducts to a specific site, such as the salivary glands or pancreas (digestive enzymes).
Hormone: A chemical messenger secreted by endocrine glands into the bloodstream that binds to specific receptors on target cells to regulate physiological activity.
Hormonal Communication
Hormonal communication depends on the ability of a hormone to interact specifically with its target cells. Each hormone affects only those cells possessing complementary receptor molecules for that hormone.
Target Cells and Receptors
Target cells contain receptor proteins embedded in their plasma membranes or within their cytoplasm/nucleus.
The hormone–receptor interaction follows a ‘lock-and-key’ mechanism: only hormones with the correct shape can bind to the receptor, ensuring specificity.
Groups of target cells responding to the same hormone form a target tissue, e.g. liver cells responding to insulin.
When a hormone binds to its receptor, it triggers a signal transduction pathway that alters cell metabolism, gene expression, or membrane permeability, depending on the hormone’s chemical nature.
Types of Hormones
Hormones fall into two main categories based on their solubility and chemical composition:
1. Peptide and Protein Hormones
These are hydrophilic (water-soluble) molecules made of amino acids, such as insulin, glucagon, and adrenaline (derived from amino acids). They cannot diffuse through the lipid bilayer of the target cell membrane.
They bind to extracellular receptors on the cell surface.
The receptor–hormone complex activates second messenger systems, such as cyclic AMP (cAMP), which then influences intracellular processes.
Second Messenger: A molecule that relays signals received at cell surface receptors to target molecules within the cell, amplifying the hormonal signal.
The cAMP pathway is a classic example of signal amplification: one hormone molecule can generate many cAMP molecules, greatly magnifying the response.
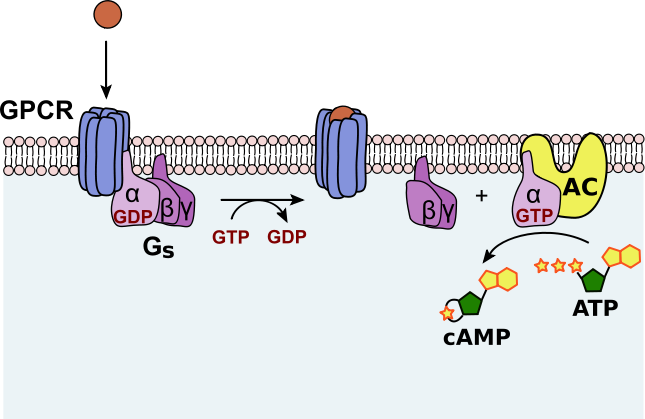
Schematic of GPCR activation of Gs, stimulation of adenylyl cyclase, and conversion of ATP to cAMP. The diagram emphasises receptor specificity at the membrane and second-messenger signal amplification inside the cell. Details beyond the core OCR scope (e.g. explicit βγ subunits) are included but remain helpful orientation. Source.
2. Steroid Hormones
Steroid hormones, such as oestrogen, progesterone, and cortisol, are lipophilic (fat-soluble) molecules derived from cholesterol. They can easily cross the phospholipid bilayer of target cells.
They bind to intracellular receptors in the cytoplasm or nucleus.
The hormone–receptor complex acts directly as a transcription factor, regulating gene expression and protein synthesis.
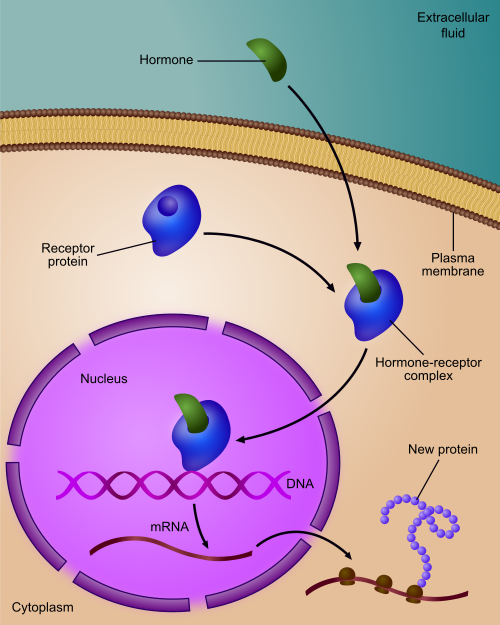
Diagram of a steroid hormone–receptor complex binding DNA and regulating transcription in target cells. It captures the slower, longer-lasting genomic mechanism compared with peptide hormones. Minor extras (e.g. co-regulators) may be implied by icons but the core pathway matches OCR requirements. Source.
This slower but longer-lasting mechanism explains why steroid hormones often have prolonged physiological effects compared with peptide hormones.
Mechanisms of Hormone Action
Peptide Hormone Mechanism (Example: Adrenaline)
Adrenaline binds to a receptor on the plasma membrane of a liver or muscle cell.
The receptor activates an enzyme, adenylyl cyclase, via a G protein.
Adenylyl cyclase converts ATP into cyclic AMP (cAMP), the second messenger.
cAMP activates a series of enzymes (protein kinases) that catalyse the conversion of glycogen to glucose.
This increases blood glucose concentration for immediate energy release during stress.
EQUATION
—-----------------------------------------------------------------
cAMP Production: ATP → cAMP + PPi
ATP = Adenosine triphosphate, energy molecule of the cell
cAMP = Cyclic adenosine monophosphate, second messenger
PPi = Inorganic pyrophosphate, by-product
—-----------------------------------------------------------------
Steroid Hormone Mechanism (Example: Oestrogen)
Oestrogen diffuses across the cell membrane.
It binds to a complementary receptor in the cytoplasm forming a hormone–receptor complex.
The complex enters the nucleus and binds to DNA promoter regions.
This stimulates or inhibits transcription of specific genes, altering protein synthesis.
Endocrine Gland Examples
The Pituitary Gland
Known as the ‘master gland’, it regulates other endocrine glands through secretion of trophic hormones such as adrenocorticotropic hormone (ACTH) and thyroid-stimulating hormone (TSH). These stimulate hormone release from the adrenal cortex and thyroid gland, respectively.
The Thyroid Gland
Secretes thyroxine (T₄) and triiodothyronine (T₃), hormones that regulate metabolic rate, growth, and development. Thyroid hormone production is controlled via negative feedback to maintain stable blood hormone concentrations.
The Adrenal Glands
Comprise two regions:
Adrenal cortex: produces steroid hormones (e.g. cortisol, aldosterone) for long-term stress and salt balance.
Adrenal medulla: secretes adrenaline and noradrenaline, peptide hormones for short-term stress responses (fight or flight).
The Pancreas (Islets of Langerhans)
Functions as both an endocrine and exocrine organ. The β-cells secrete insulin to lower blood glucose, while α-cells secrete glucagon to raise it, maintaining glucose homeostasis.
The Gonads
Ovaries secrete oestrogen and progesterone, regulating female reproductive cycles and secondary sexual characteristics.
Testes produce testosterone, responsible for male reproductive development and muscle growth.
Control and Feedback
Hormone secretion is tightly regulated by negative feedback loops, ensuring homeostasis. For instance:
High blood thyroxine levels inhibit TSH release from the pituitary.
Low blood glucose triggers glucagon secretion, while high glucose promotes insulin release.
Positive feedback occurs less commonly but can amplify specific processes, such as oxytocin release during childbirth contractions.
Summary of Key Features of Endocrine Communication
Slow onset, long duration, and widespread effects compared with neural control.
Specificity achieved through receptor–hormone complementarity.
Integration with the nervous system via the hypothalamus–pituitary axis, which coordinates overall body responses to maintain internal equilibrium.
FAQ
The hypothalamus acts as the link between the nervous and endocrine systems. It monitors internal conditions such as temperature and blood composition, then releases releasing or inhibiting hormones to control the pituitary gland.
For example:
Thyrotropin-releasing hormone (TRH) stimulates the pituitary to release TSH, which then acts on the thyroid gland.
Corticotropin-releasing hormone (CRH) triggers ACTH secretion, influencing adrenal cortex activity.
This integration allows the hypothalamus to maintain homeostasis through both neural and hormonal control.
Hormones differ in their solubility, target mechanism, and rate of breakdown.
Steroid hormones are lipid-soluble and alter gene transcription, meaning their effects last longer because new proteins are synthesised and remain active for hours or days.
Peptide hormones act through second messengers, leading to faster but shorter-lived effects as enzymes are rapidly degraded or inactivated.
The body’s need for rapid or sustained regulation determines which hormone type predominates in a given pathway.
To avoid overstimulation, the body employs several control mechanisms:
Negative feedback loops, where rising hormone levels inhibit further release (e.g. thyroxine on TSH).
Receptor downregulation, reducing the number of active receptors on target cells after prolonged exposure.
Hormone degradation by enzymes in the liver or kidneys to limit active hormone duration.
These processes ensure that hormone action remains balanced and responsive to changing internal conditions.
Hormone secretion can fluctuate due to several physiological and environmental factors:
Circadian rhythms – e.g. cortisol peaks in the early morning.
Stress and emotion, which increase secretion of adrenaline and cortisol.
Nutrient levels, such as glucose concentration affecting insulin and glucagon.
Other hormones, where one hormone may promote or inhibit another’s release (e.g. hypothalamic control of pituitary hormones).
These dynamic controls ensure hormones are secreted precisely when needed.
If receptors are absent or defective, the target cell becomes hormone-insensitive, disrupting normal regulation.
For instance:
Faulty insulin receptors can cause Type 2 diabetes mellitus, where cells fail to respond to insulin even when levels are normal or high.
Mutations in thyroid hormone receptors can lead to metabolic disorders due to lack of cellular response.
This demonstrates that hormone effectiveness depends not just on secretion but also on correct receptor function.
Practice Questions
Question 1 (2 marks)
Explain the difference between endocrine and exocrine glands.
Mark scheme:
1 mark for stating that endocrine glands secrete hormones directly into the bloodstream (no ducts).
1 mark for stating that exocrine glands secrete substances through ducts to a specific site (e.g. salivary glands, pancreas for digestive enzymes).
Question 2 (5 marks)
Describe how peptide hormones and steroid hormones differ in their mechanisms of action on target cells.
Mark scheme:
Award up to 5 marks for the following points (1 mark each):
Peptide hormones are hydrophilic and cannot pass through the cell membrane.
They bind to receptors on the cell surface membrane, forming a hormone–receptor complex.
The receptor activates a second messenger system (e.g. cAMP) that brings about intracellular changes.
Steroid hormones are lipophilic and diffuse through the phospholipid bilayer.
They bind to intracellular receptors in the cytoplasm or nucleus to form a hormone–receptor complex, which acts as a transcription factor to alter gene expression.

